About Adult Tube Feeding
If an adult patient has a functioning gastrointestinal tract but is unable to ingest adequate nutrients by mouth, enteral nutrition is an option.1 Enteral nutrition is preferred over parenteral nutrition since it helps preserve GI function, allowing normal absorption of nutrients in the digestive tract.5
Enteral nutrition helps patients who are nutritionally depleted or at risk for becoming depleted by delivering important nutrients when they might otherwise be unable or unwilling to consume what they need. There are many clinical reasons in which enteral nutrition may be warranted, including: 6
- Feeding and swallowing disorders
- Food allergies
- Cancer
- Gastrointestinal issues such as an obstructed bowel, short bowel syndrome, or Crohn’s disease
- Excessive nutrient losses through diarrhea, vomiting or fistulae
- Gastroesophageal reflux disease (GERD) or esophagitis
- Neurological disorders including paralysis
- Recovery from surgery or trauma
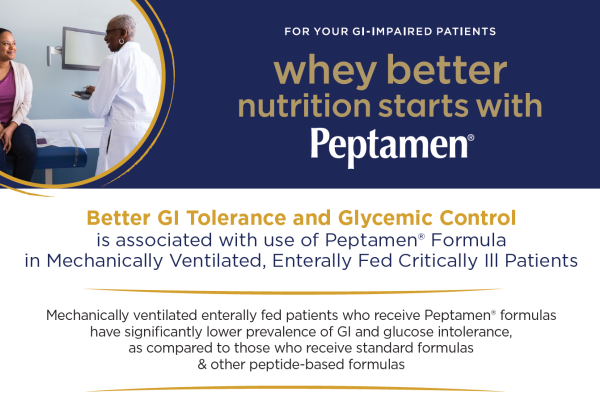
- Critical illnesses requiring mechanical ventilation
Enteral nutrition may be done through the nose or directly into the GI tract. The type varies based on the patient’s clinical condition as well as the approximate duration of enteral nutrition as nutrition therapy. For example:
- Nasoenteral are enteral feeding tubes placed in the nose that empty either into the stomach [nasogastric (NG)] or intestines [nasoduodenal (ND)/nasojejunal (NJ)]. These enteral nutrition routes are often used when nutrition support is meant to be for a shorter duration, such as 4-6 weeks or less.
- Gastrostomy is a procedure in which the feeding tube (i.e., G-tube or PEG, for percutaneous endoscopic gastrostomy) is placed directly into the stomach. Patients with a gastrostomy tube often need it for a longer period of time.
- Jejunostomy is when the tube (i.e., J-tube) is placed directly into the jejunum of the small intestine. These can be used if the patient is at a higher risk of aspiration, or if the patient has had previous gastric surgery.
Nestlé Health Science has a variety of enteral tube feeding formulas that can be used for any type of enteral nutrition or nourishment regimen, including bolus feedings (larger feedings administered several times a day, similar to meals and snacks), or as part of a continuous feeding (a much smaller volume is delivered at a constant rate for up to 24 hours a day).
Nutrition & Adult Tube Feeding
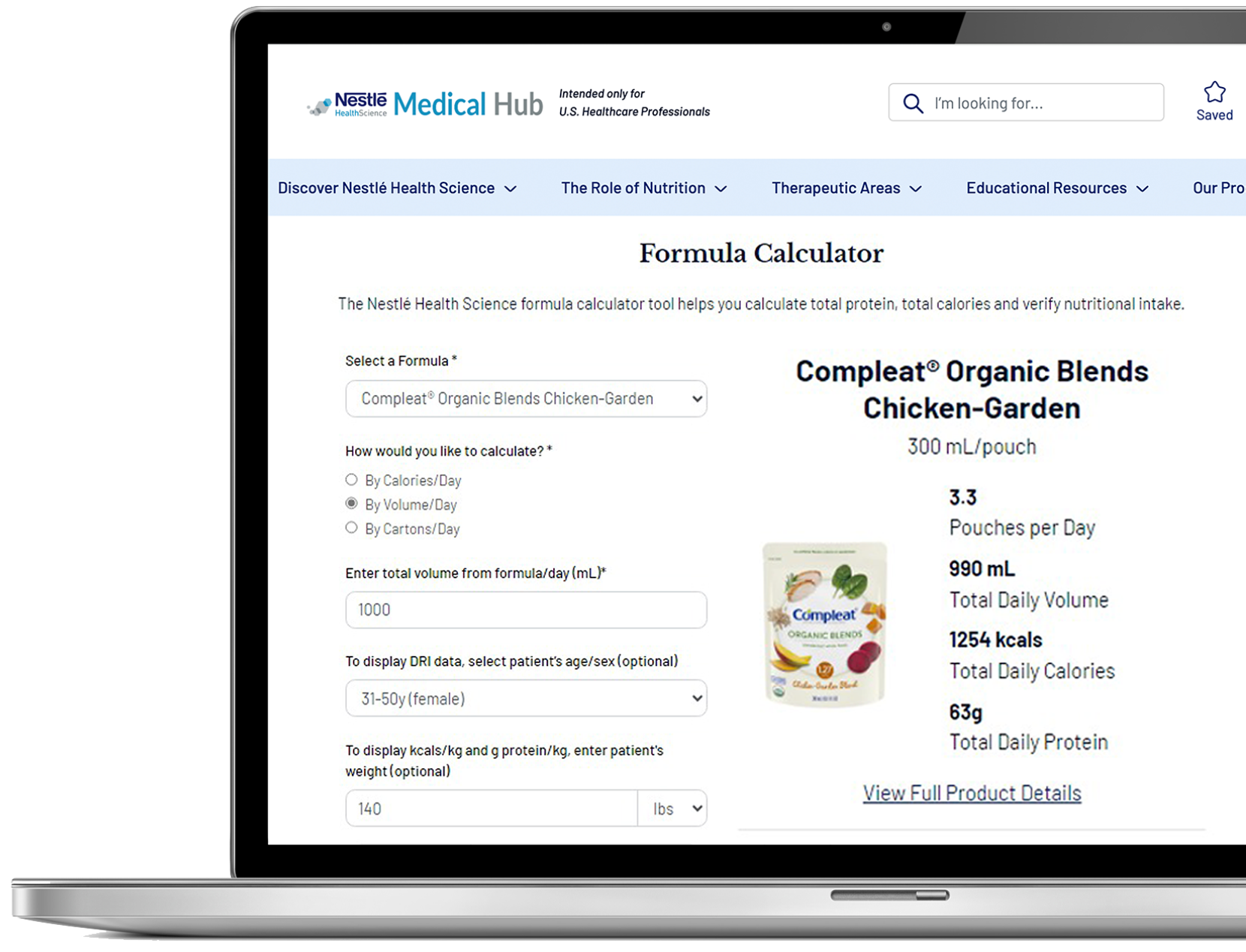
When it comes to determining the nutrition and formula needs for patients receiving enteral nutrition, there are a number of considerations.7 A general guideline is to provide a patient with 12-25 calories per kilogram of body weight per day (12-25 kcal/kg/day) using a standard feeding formula. 8 The dietitian and healthcare team will determine the right combination of nutrients, calories, and fluid amounts that are appropriate for the individual patient.
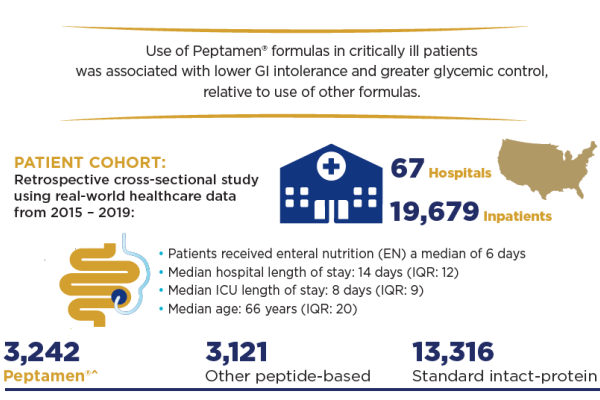
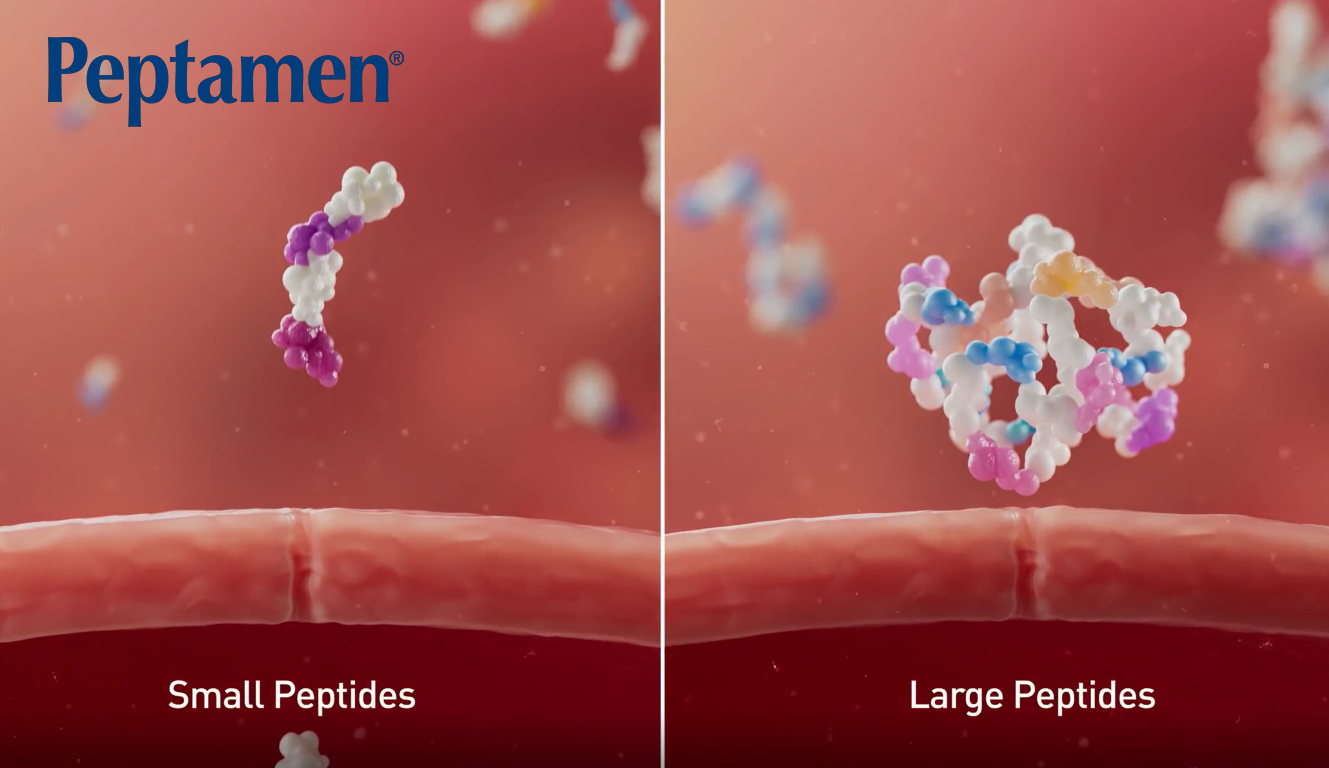
There are several types of tube feeding formulas available to meet the needs of adults requiring enteral nutrition. The majority likely can tolerate a standard intact protein formula, but depending on the patient’s condition, there are times when a specialized formula is needed.
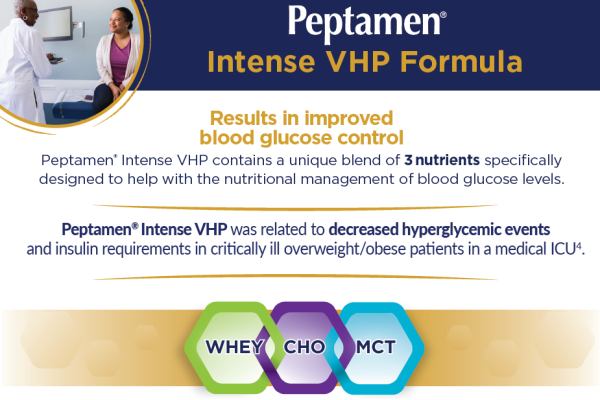
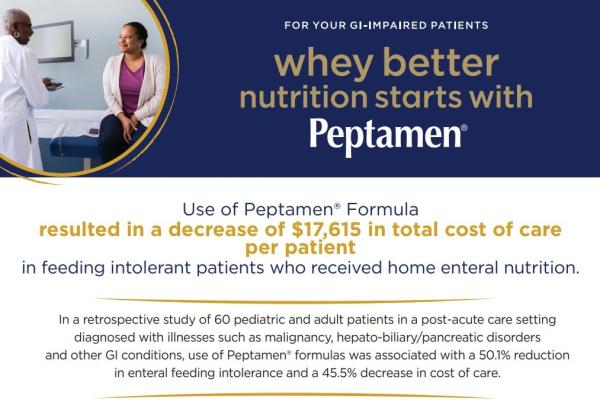
Nestlé Health Science offers a comprehensive portfolio of high-quality, evidence-based enteral tube feeding formulas to meet the needs of adults receiving enteral nutrition. Our portfolio includes:
- Standard formulas for normal digestion
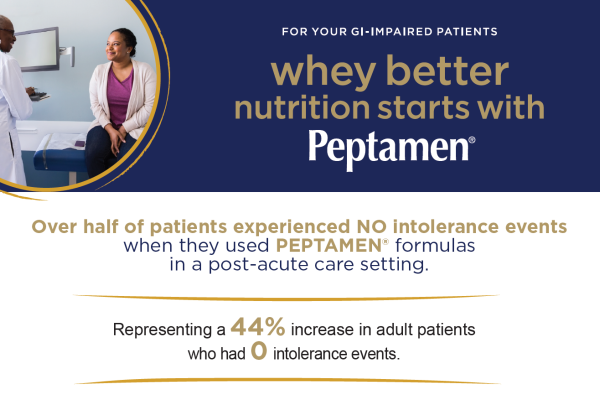
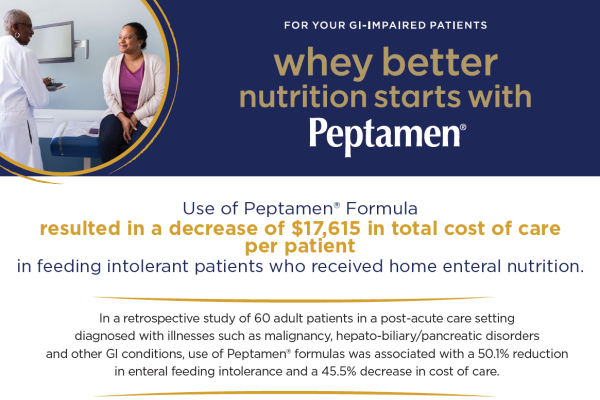
- Peptide-based formulas for gastrointestinal intolerance
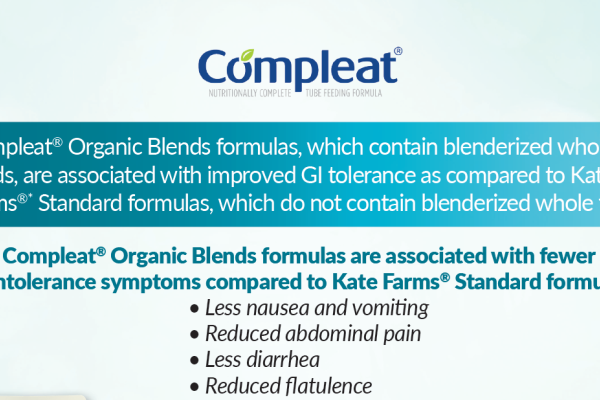
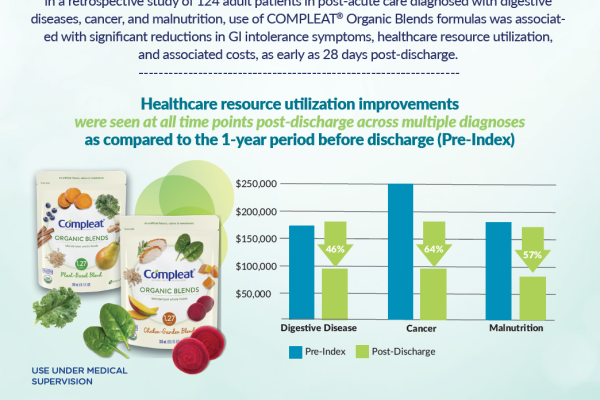
- Formulas containing real food ingredients to support feeding tolerance and variety
These formulas meet the highest standards of nutritional quality, supporting overall improved outcomes.
Support Resources
You must be logged in to view all resources.
31 Evidence Found
23 Tools and Product Support Found
11 Patient Resources Found
27 Videos
References
-
https://www.nutritioncare.org/About_Clinical_Nutrition/What_Is_Enteral_Nutrition_/
-
https://www.nutritioncare.org/about_clinical_nutrition/nutrition_support_patient_data_fact_sheet/
-
Singer P et al. ESPEN Practical and Partially Revised Guideline: Clinical Nutrition in the Intensive Care Unit. Clin Nutr 2023; 42: 1671-1689.
-
Bechtold M et al. When Is Enteral Nutrition Indicated? J Parenter Enteral Nutr. 2022; 46:1470-1496. doi:10.1002/jpen.2364
-
Compher C, Bingham AL, McCall M, et al. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition. J Parenter Enteral Nutr. 2022; 46: 12–41. https://doi.org/10.1002/jpen.2267
-
Epp L, Blackmer A, Church A, Ford I, Grenda B, Larimer C, Lewis-Ayalloore J, Malone A, Pataki L, Rempel G, Washington V; ASPEN Enteral Nutrition Committee. Blenderized tube feedings: Practice recommendations from the American Society for Parenteral and Enteral Nutrition. Nutr Clin Pract. 2023 Dec; 38(6): 1190-1219. doi: 10.1002/ncp.11055. Epub 2023 Oct 3. PMID: 37787762.