About Dysphagia
Dysphagia is a medical condition that affects a patient's ability to swallow properly. It can occur at any stage of life, from infancy to the older adult, and can result from a wide range of causes such as neurological disorders, structural abnormalities, or other medical conditions that affect the mouth, throat or esophagus. Dysphagia can cause significant physical and emotional distress, contributing to choking, aspiration, and malnutrition.
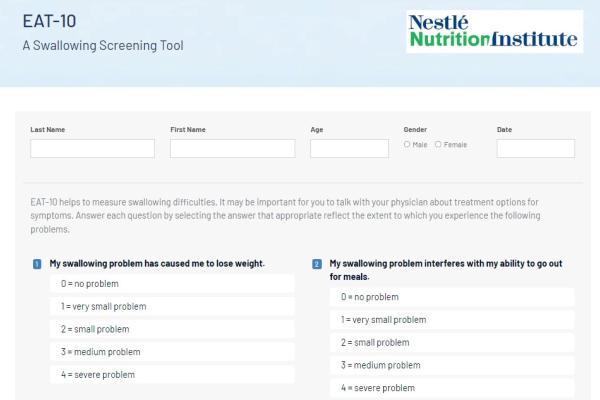
Healthcare Professionals play an important role in identifying and managing dysphagia in their patients. Symptoms of dysphagia may include coughing or choking during meals, difficulty swallowing food and/or liquids, and regurgitation. Speech Language Pathologists (SLP) often conduct a bedside swallow screen as the initial assessment and proceed as appropriate with diagnostic tests such as a Videofluoroscopic Swallow Study (VFSS), Fiberoptic Endoscopic Evaluation of Swallow (FEES) or High-Resolution Manometry (HRM). SLPs and/or physicians may evaluate swallowing with an upper endoscopy procedure to identify the cause of dysphagia. Treatment may involve dietary modifications, swallowing therapy, medication, or surgery depending on the underlying cause and severity of the condition. Early recognition and proper management of dysphagia can improve quality of life, reduce the risk of complications such as aspiration pneumonia, and help patients achieve optimal nutrition status.
Nutrition & Dysphagia
Patients with dysphagia often face challenges in maintaining adequate nutrition due to their difficulties in swallowing. This can lead to malnutrition, dehydration, and an increased risk of aspiration pneumonia. Registered Dietitians play a key role in identifying patients with or at risk of dysphagia. Early identification is important for timely referrals to a Speech Language Pathologist who evaluates the swallow to identify the appropriate modified texture of food and liquid and whether other treatments are necessary to help improve swallowing function and reduce the risk of aspiration. Registered Dietitians manage the nutritional needs of patients with dysphagia to provide optimal nutrition and hydration.
Nutritional Strategies for Dysphagia
Managing the nutritional needs of patients with dysphagia is critical for their overall health and well-being.
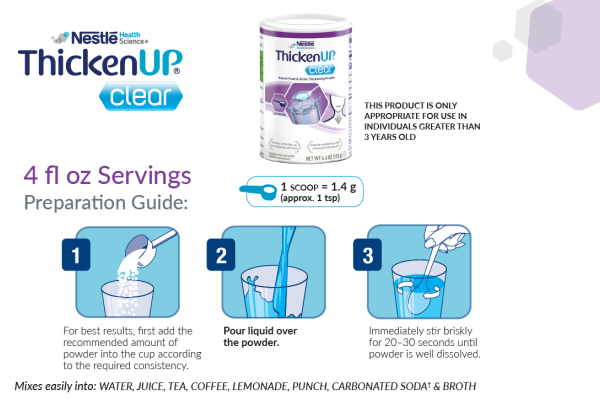
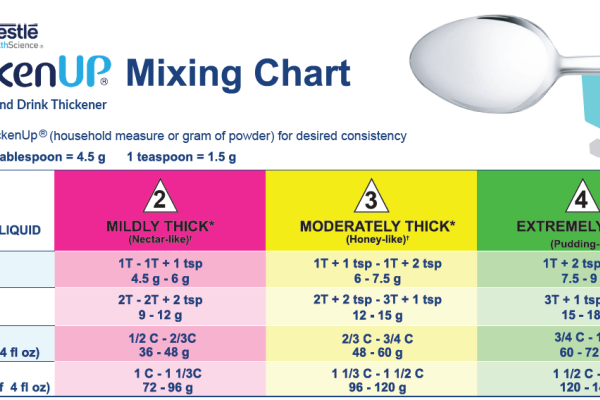
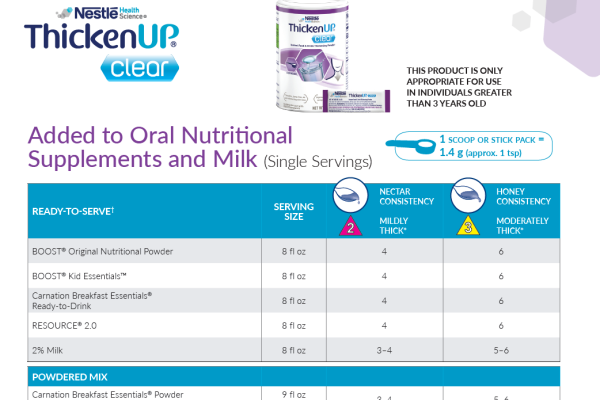
One of the primary nutrition strategies used in the treatment of dysphagia is modifying the texture of food and liquids.* This involves altering the consistency of food and drinks to make them easier to swallow. For example, foods can be pureed, minced, softened, or chopped into bite-sized pieces, while liquids can be thickened to make the bolus easier to control in the mouth and swallow. Swallowing is evaluated by a Speech Language Pathologist who identifies the type of texture modification required for a safer swallow. This can often involve a combination of different techniques to promote optimal nutrition.
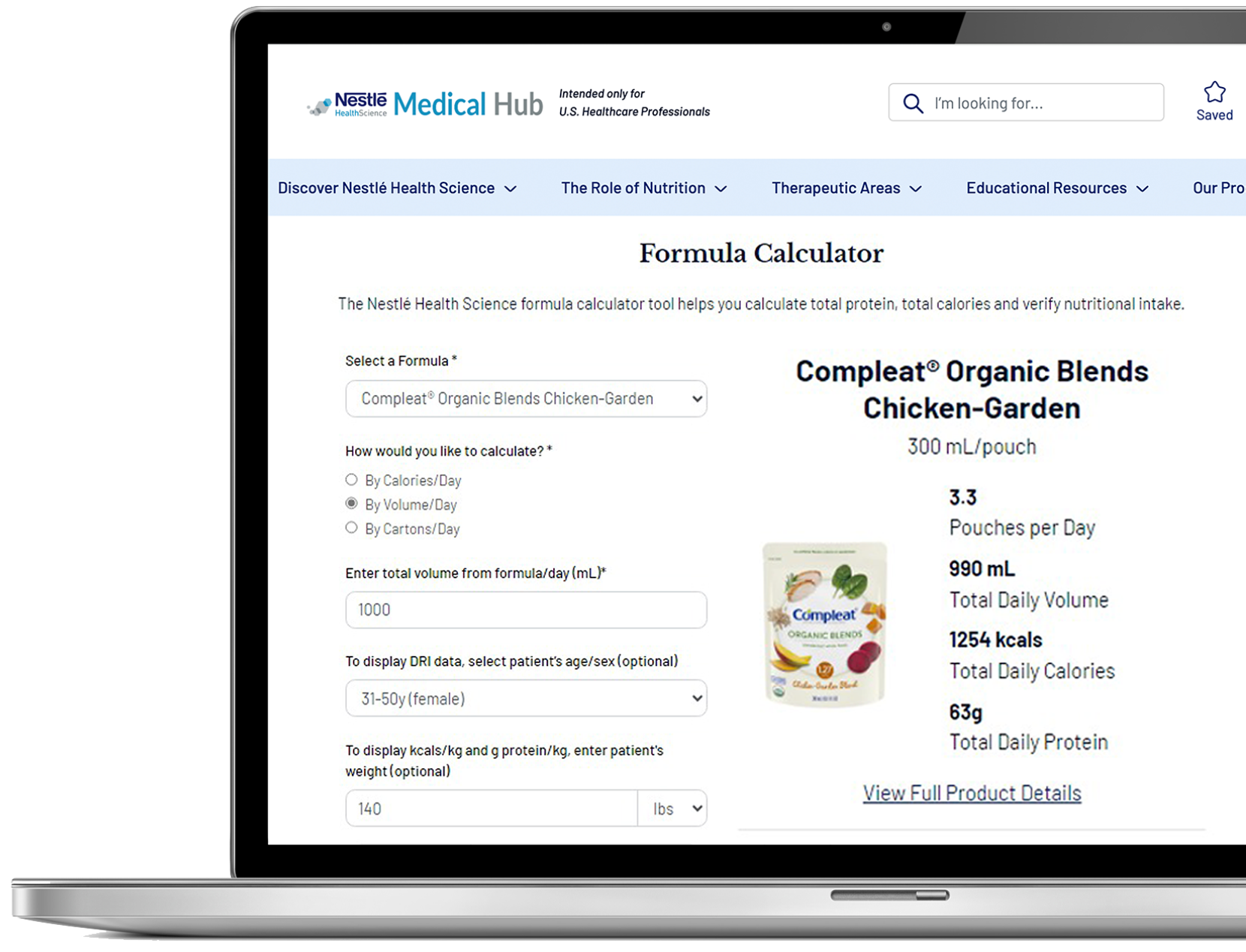
Another key strategy in the management of dysphagia patients is to minimize the risk of malnutrition and dehydration. Providing appropriate nutritional therapy, such as oral supplements or tube feeding, can help to meet 100% of estimated needs when not met by diet alone. Registered Dietitians work with patients and their families to develop a customized nutrition plan that meets the patient's specific needs, preferences, and goals.
*Learn more about texture modification at IDDSI.org
Support Resources
You must be logged in to view all resources.
7 Tools and Product Support Found
5 Patient Resources Found
2 Videos
References
1. Bhattacharyya N. The prevalence of dysphagia among adults in the United States. Otolaryngology Head and Neck Surgery. 2014;151(5):765-769.
2. Adkins C, Takakura W, Spiegel BMR, et al. Prevalence and characteristics of dysphagia based on a population-based survey. Clin Gastroenterol Hepatol. 2020;18(9):1970-1979.
3. Yarrow L and Mertz Garcia J. Malnutrition: Risks & concerns in dysphagia management. Dysphagia. 2010;19(4):115-120.