About Obesity
Obesity is a growing public health concern. According to the CDC, nearly 1 in 3 adults (30.7%) are overweight and 42.4% are obese. This includes 9.2% who are classified as severely obese.4
Obesity is a chronic disease strongly linked to conditions including type 2 diabetes, hypertension, stroke, metabolic syndrome, obstructive sleep apnea, Non-Alcoholic Fatty Liver Disease (NAFLD), Non-Alcoholic Steatohepatitis (NASH), coronary heart disease and osteoarthritis. Modest sustained body weight loss ranging from 5 – 15% is likely to result in clinically meaningful health benefits in individuals with those conditions.5
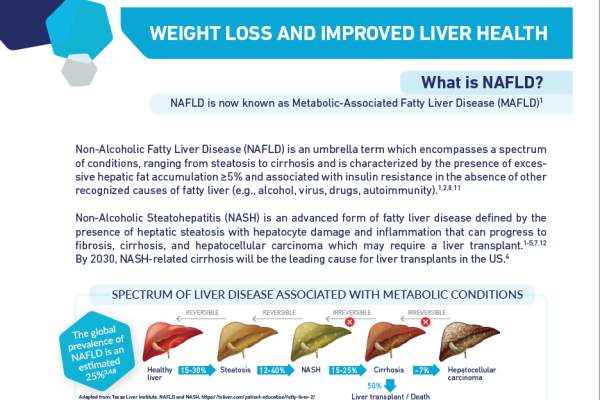
OBESITY AND LIVER DISEASE
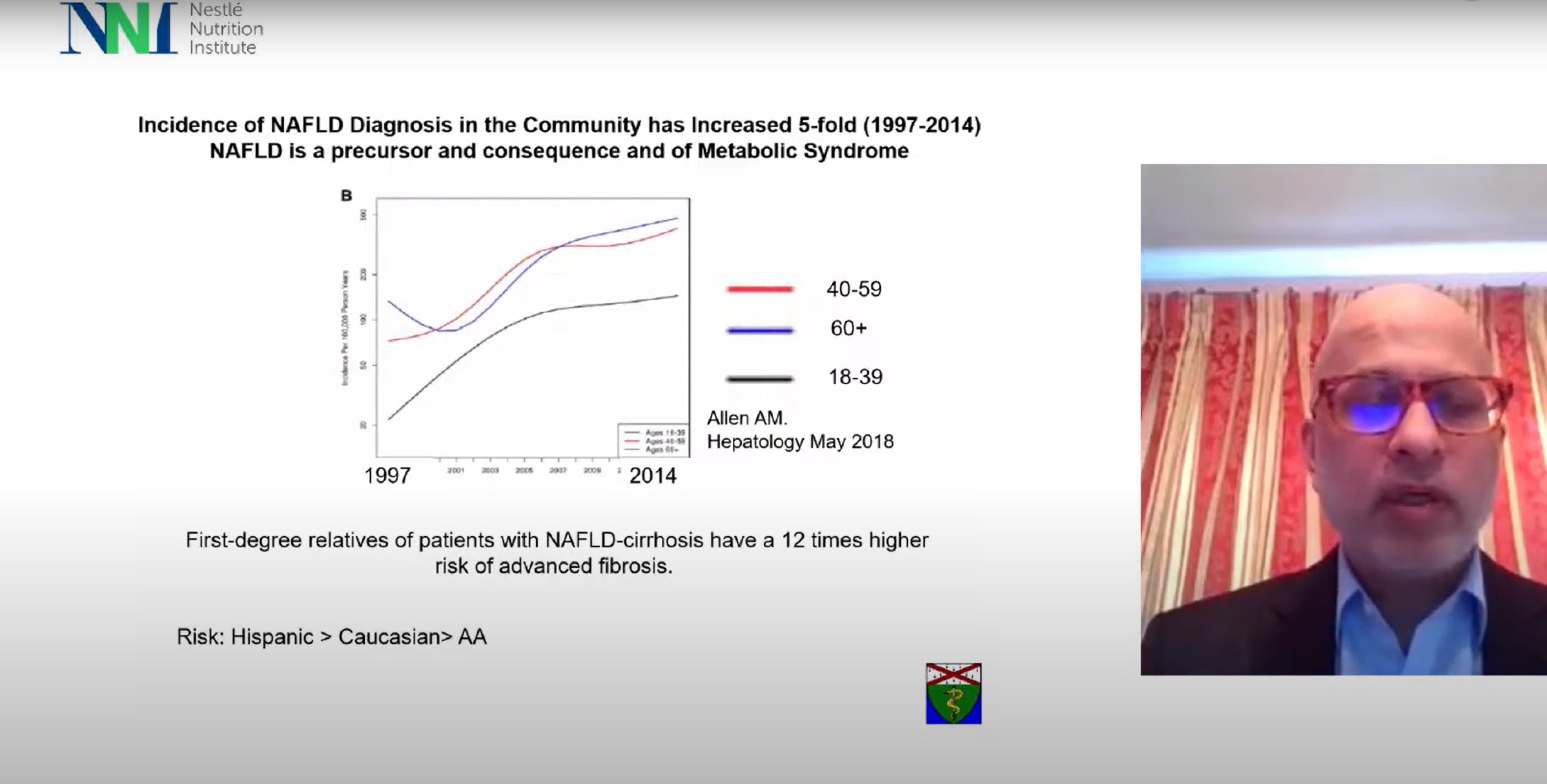
Non-Alcoholic Fatty Liver Disease (NAFLD) and its advanced stage, Non-Alcoholic Steatohepatitis (NASH), are becoming increasingly prevalent, affecting an estimated 30% and 5% respectively, of people worldwide and presenting significant health challenges.6 NAFLD encompasses a spectrum of conditions, ranging from steatosis to cirrhosis7 and is characterized by the presence of excessive hepatic fat accumulation ≥5%8 and associated with insulin resistance in the absence of other recognized causes of fatty liver (e.g., alcohol, virus, drugs, autoimmunity).7
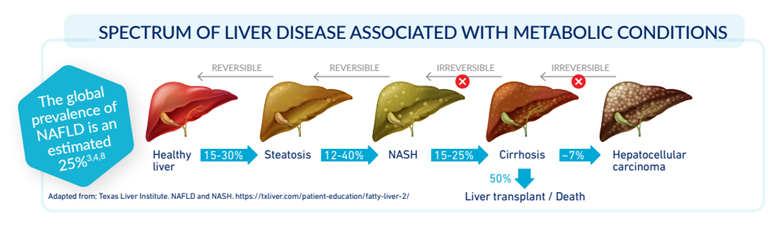
There are no approved pharmacological interventions available for NAFLD7,8,9, however emerging research has shown that weight loss of at least +10% can have profound effects on these conditions. Shedding excess weight through a balanced approach of dietary modifications and regular physical activity has demonstrated the potential to reverse liver fat accumulation, inflammation, and fibrosis.10 As healthcare professionals, understanding the intricate interplay between weight loss and liver health is paramount in guiding patients towards improved outcomes and fostering healthier futures.
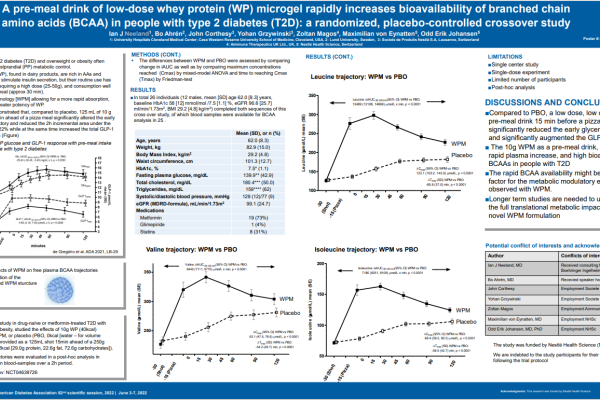
OBESITY AND TYPE 2 DIABETES
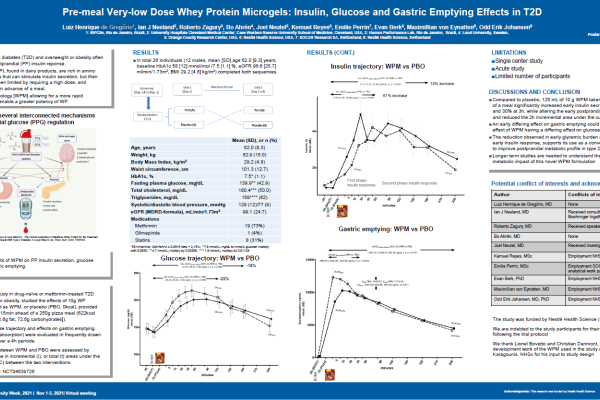
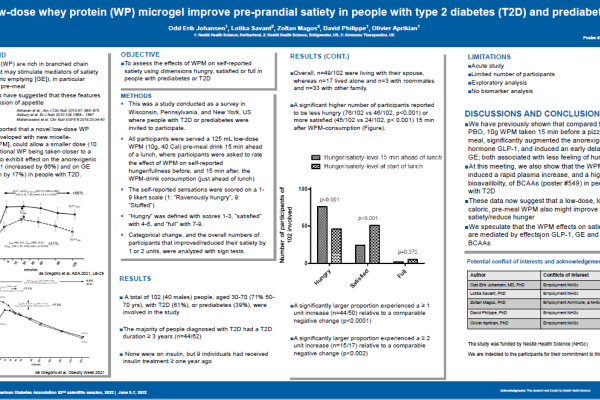
Obesity, particularly excess abdominal fat, triggers insulin resistance, leading to impaired glucose regulation. As a result, individuals with obesity face a substantially heightened risk of developing type 2 diabetes (T2DM).11
One out of nine individuals in the US population (37 million people) have diabetes. Most of them are diagnosed with T2DM.12
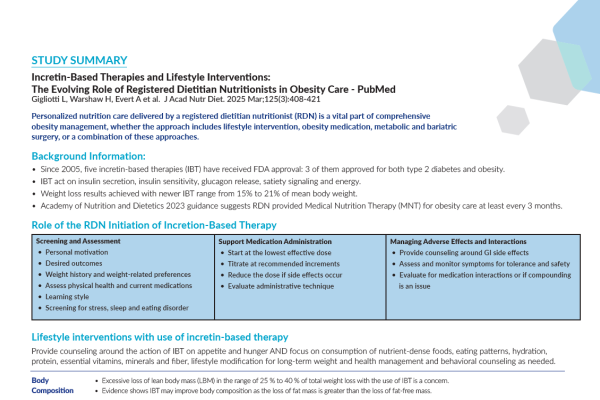
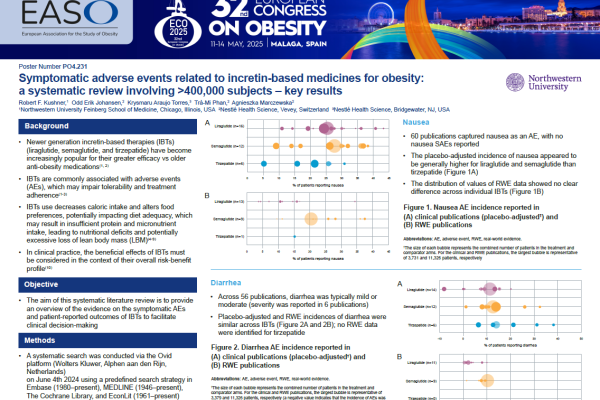
However, by reducing obesity through evidence-based weight-loss strategies such as lifestyle modifications, personalized nutrition or diet replacement programs, and increased physical activity, healthcare professionals can empower patients to significantly reduce their risk of type 2 diabetes and its associated complications.13,14,15,16,17,18
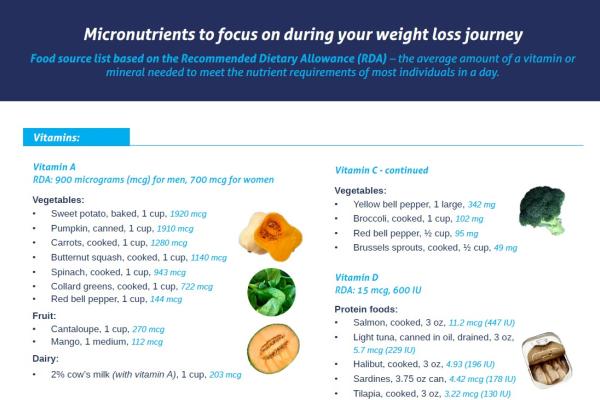
Nutrition & OBESITY
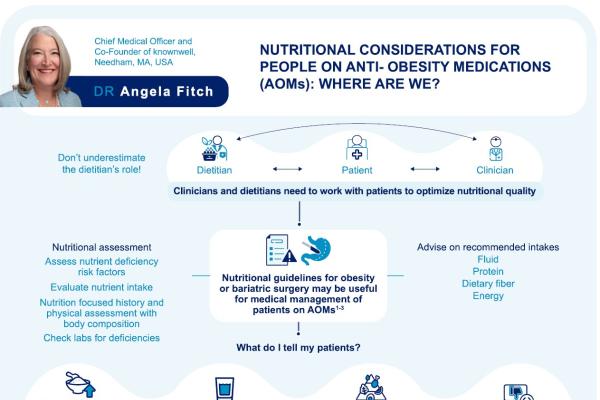
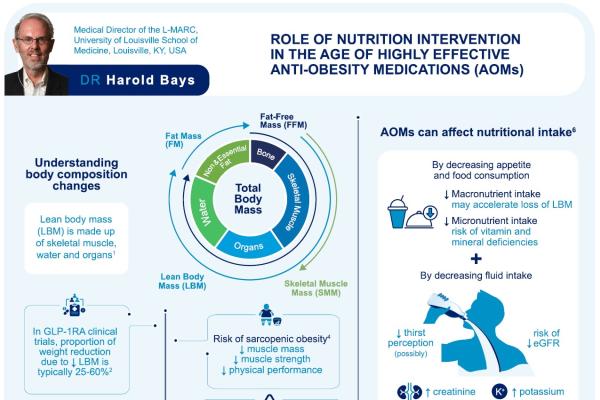
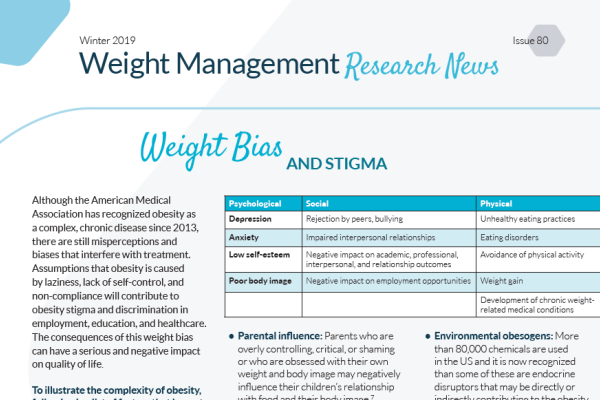
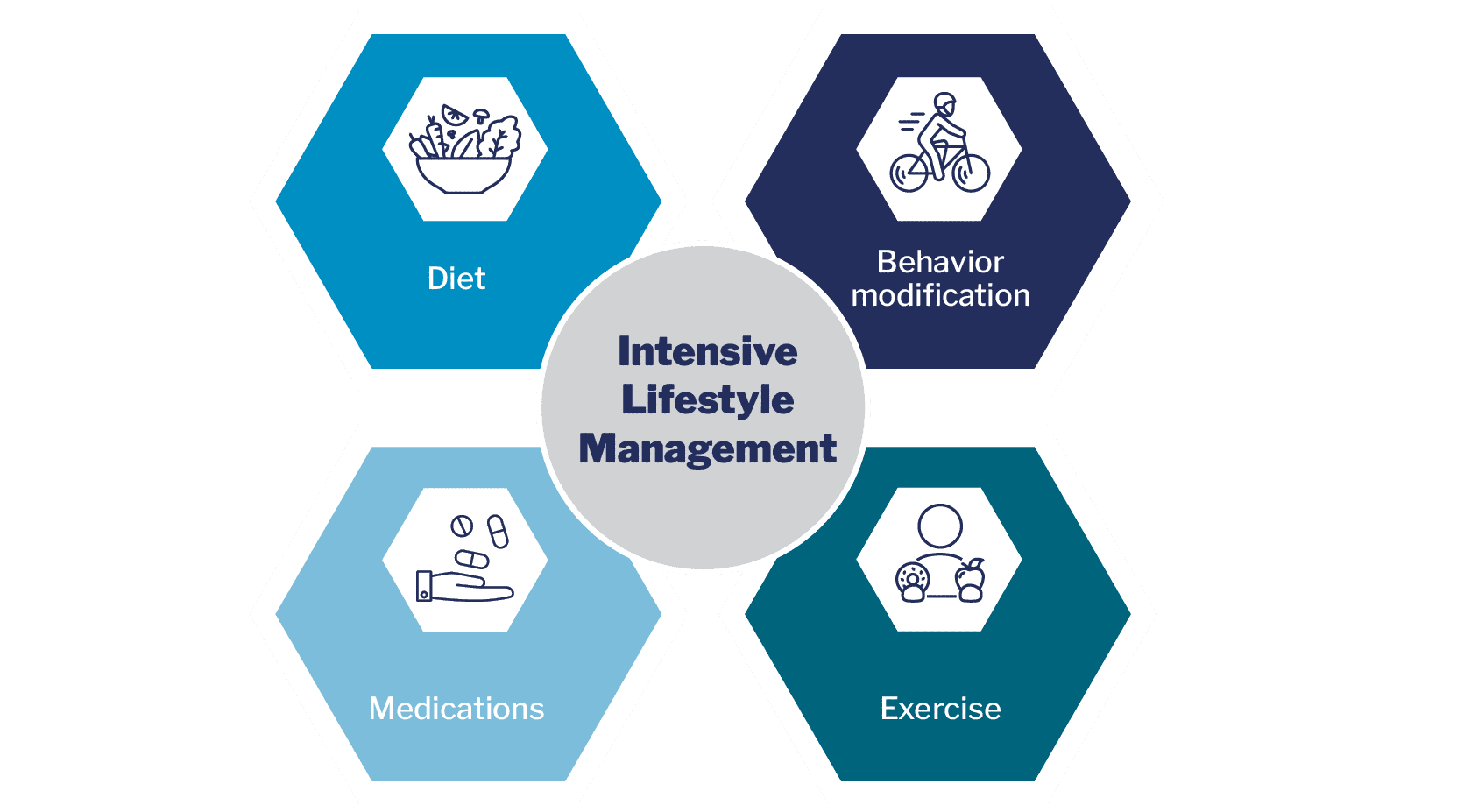
While there is no single approach to treating obesity, experts agree that the first step toward achievement of successful weight loss and maintenance is a comprehensive lifestyle approach that includes dietary modification, physical activity and behavioral therapy.8,9,19
NUTRITION STRATEGIES FOR OVERWEIGHT PATIENTS (BMI 25-29.9)
For overweight patients, a balanced approach to nutrition management is often appropriate. Emphasizing the importance of a well-rounded, nutritious diet can help patients achieve gradual weight loss while building healthy habits for the long term. Encouraging portion control, mindful eating, and incorporating regular physical activity can further complement these efforts. Meal replacement programs, consisting of nutritionally formulated shakes or bars, may be considered as adjuncts to conventional dietary strategies. These programs can provide convenient and structured options that help patients control their caloric intake while ensuring essential nutrient requirements are met. Close monitoring and personalized support from healthcare providers are essential for sustainable success in this population.
NUTRITION STRATEGIES FOR OBESE PATIENTS (BMI 30+)
Obese and severely obese patients may face more complex challenges that require a more comprehensive weight-loss approach. Meal replacement programs, under proper medical supervision, can be a valuable tool in the initial phase of weight loss for severely obese individuals. These programs may help to rapidly reduce caloric intake, which can be motivating for patients, facilitate significant weight loss20, and can help reduce blood glucose levels.21,22
However, due to the severity of obesity and potential underlying health issues, a multidisciplinary approach can be most effective. Collaboration between dietitians, psychologists, and other healthcare specialists can address psychological and behavioral factors related to overeating, enabling long-term success. Additionally, emphasizing behavior modification, setting realistic goals, and encouraging increased physical activity can foster lasting lifestyle changes that support sustained weight loss and overall well-being.
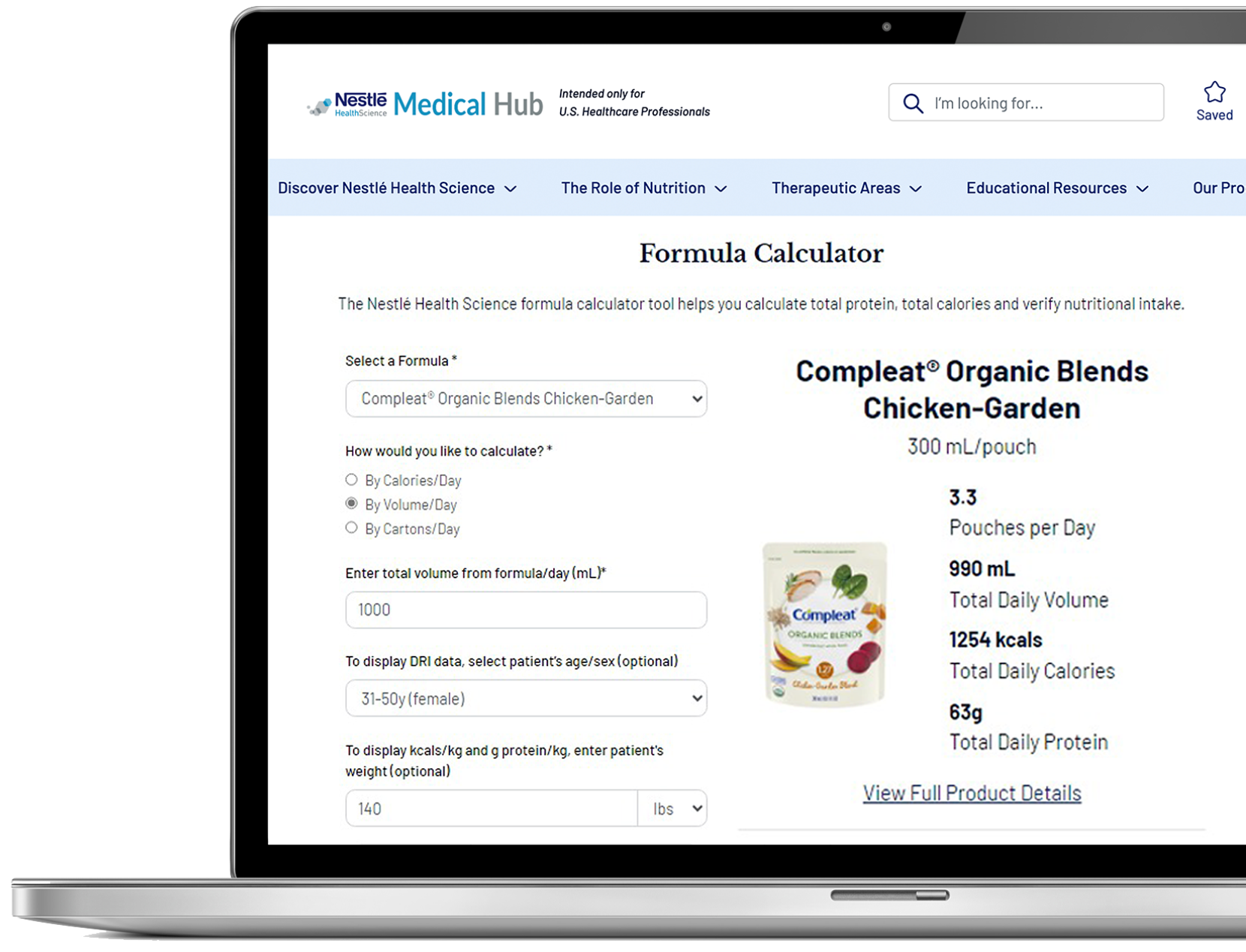
At Nestlé Health Science, we collaborate with key opinion leaders, healthcare providers, and researchers to develop nutritional solutions for weight management and associated health conditions. Through extensive research and innovation, we have created tailored programs, products, and meal replacements that empower patients to achieve lasting results and improved overall health.
Support Resources
You must be logged in to view all resources.
19 Evidence Found
8 Tools and Product Support Found
9 Patient Resources Found
11 Videos
References
1. Ward ZJ, Bleich SN, Cradock AL et al. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N Engl J Med. 2019 Dec 19;381(25):2440-2450.
2. Tiwari A, Balasundaram P. Public Health Considerations Regarding Obesity. [Updated 2023 Mar 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
3. Thorpe, K; Toles, A; Shah, Bimal et al. Weight Loss-Associated Decreases in Medical Care Expenditures for Commercially Insured Patients With Chronic Conditions. Journal of Occupational and Environmental Medicine: October 2021, 63 (10); 847-851
4. https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity
5. Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017 Jun;6(2):187-194.
6. Younossi ZM, Golabi P, Paik JM et al. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. 2023 Apr 1;77(4):1335-1347.
7. Abd El-Kader SM, El-Den Ashmawy EM. Non-alcoholic fatty liver disease: The diagnosis and management. World J Hepatol. 2015 Apr 28;7(6):846-58.
8. Karjoo S et al. Nonalcoholic fatty liver disease and obesity: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022, Obesity Pillars, Volume 3, 2022.
9. Cusi K, Isaacs S, Barb D et al. American Association of Clinical Endocrinology Clinical Practice Guideline for the Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Primary Care and Endocrinology Clinical Settings: Co-Sponsored by the American Association for the Study of Liver Diseases (AASLD). Endocr Pract. 2022 May;28(5):528-562.
10. Scragg J, Avery L, Cassidy S et al. Feasibility of a Very Low Calorie Diet to Achieve a Sustainable 10% Weight Loss in Patients With Nonalcoholic Fatty Liver Disease. Clin Transl Gastroenterol. 2020 Sep;11(9):e00231. doi: 10.14309/ctg.0000000000000231.
11. Wondmkun YT. Obesity, Insulin Resistance, and Type 2 Diabetes: Associations and Therapeutic Implications. Diabetes Metab Syndr Obes. 2020 Oct 9;13:3611-3616.
12. https://www.cdc.gov/diabetes/data/statistics-report/index.html
13. Evert AB, Dennison M, Gardner CD et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019 May;42(5):731-754.
14. Echouffo-Tcheugui JB, Selvin E. Prediabetes and What It Means: The Epidemiological Evidence. Annu Rev Public Health. 2021 Apr 1;42:59-77.
15. Lean ME et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018 Feb 10;391(10120):541-551.
16. Noronha JC, Thom G, Lean MEJ. Total Diet Replacement Within an Integrated Intensive Lifestyle Intervention for Remission of Type 2 Diabetes: Lessons From DiRECT. Front Endocrinol (Lausanne). 2022 Jun 2;13:888557.
17. Diabetes Prevention Program (DPP) Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002 Dec;25(12):2165-71
18. Salvia MG. The Look AHEAD Trial: Translating Lessons Learned Into Clinical Practice and Further Study. Diabetes Spectr. 2017 Aug;30(3):166-170.
19. Younossi ZM, Corey KE, Lim JK. AGA Clinical Practice Update on Lifestyle Modification Using Diet and Exercise to Achieve Weight Loss in the Management of Nonalcoholic Fatty Liver Disease: Expert Review. Gastroenterology. 2021 Feb;160(3):912-918.
20. Ard JD, Lewis KH, Rothberg A, Auriemma A, Coburn SL, Cohen SS, Loper J, Matarese L, Pories WJ, Periman S. Effectiveness of a Total Meal Replacement Program (OPTIFAST Program) on Weight Loss: Results from the OPTIWIN Study. Obesity (Silver Spring). 2019 Jan;27(1):22-29.
21. Rothberg AE, Ard JD, Auriemma A et al. Effect of Total Meal Replacement Program Compared with a Reduced-Energy Food-Based Diet Plan on Glycemic Status—Results from the OPTIWIN Study. Diabetes 1 July 2018; 67 (Supplement_1): 298–LB. https://doi.org/10.2337/db18-298-LB
22. Keogh JB, Clifton PM. Meal replacements for weight loss in type 2 diabetes in a community setting. J Nutr Metab. 2012;1-7. doi:10.1155/2012/918571.