About Pediatric Tube Feeding
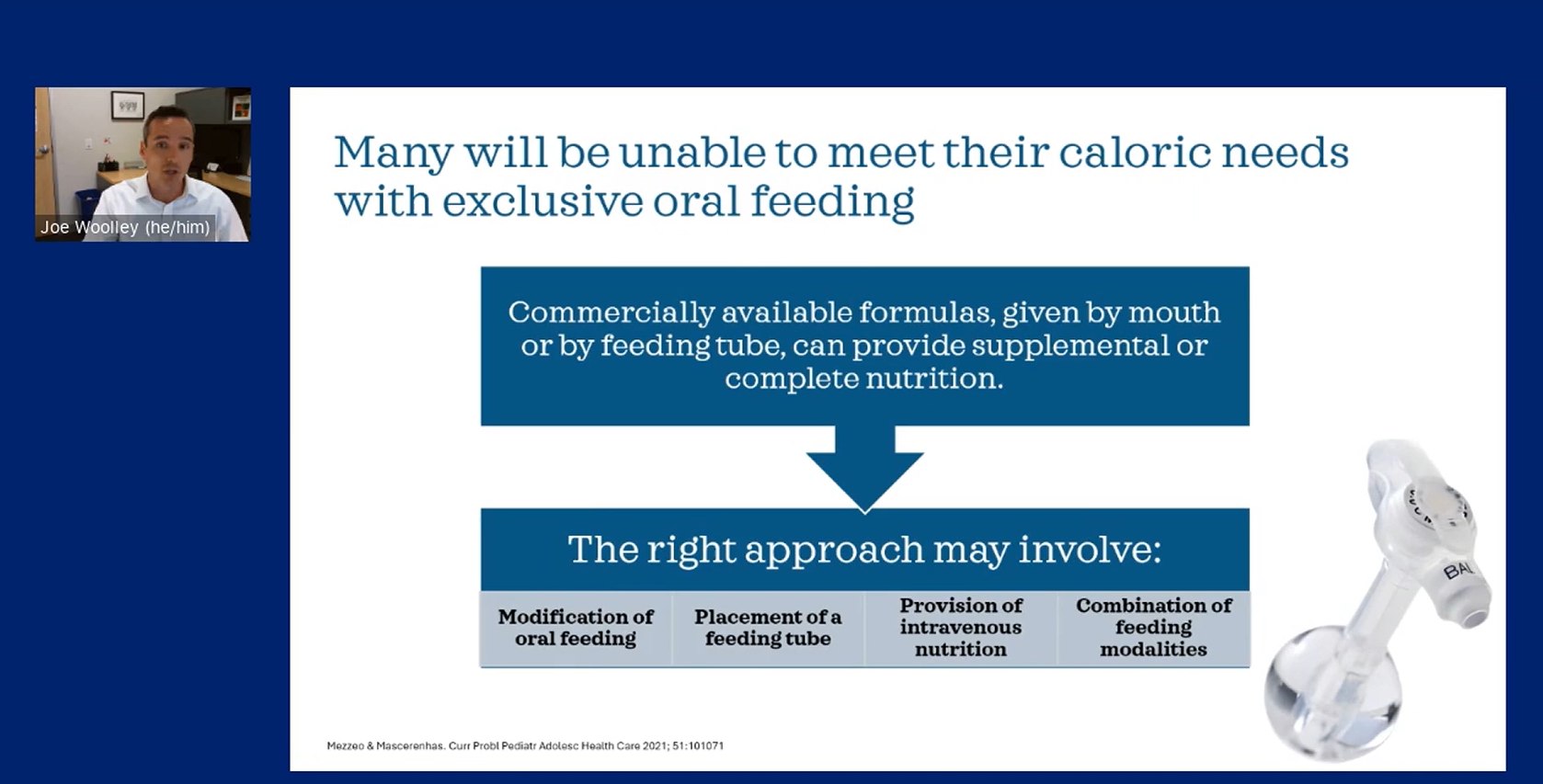
Pediatric tube feeding, also known as enteral nutrition (EN), is a way of providing essential nutrition to infants and children who are unable or unwilling to meet their dietary needs orally.1
Enteral tube feeding is commonly used in patients with feeding and swallowing disorders associated with development delays, malnutrition, diseases of the digestive tract, neurological impairment, and may also be useful for the nutritional management of other conditions such as Crohn’s disease, multiple food allergy and/or intolerance to certain foods as well as medical conditions that interfere with normal eating, digestion, or absorption of nutrients, such as gastroesophageal reflux disease (GERD), esophagitis, cystic fibrosis (CF) or other acute and chronic illnesses.2,3
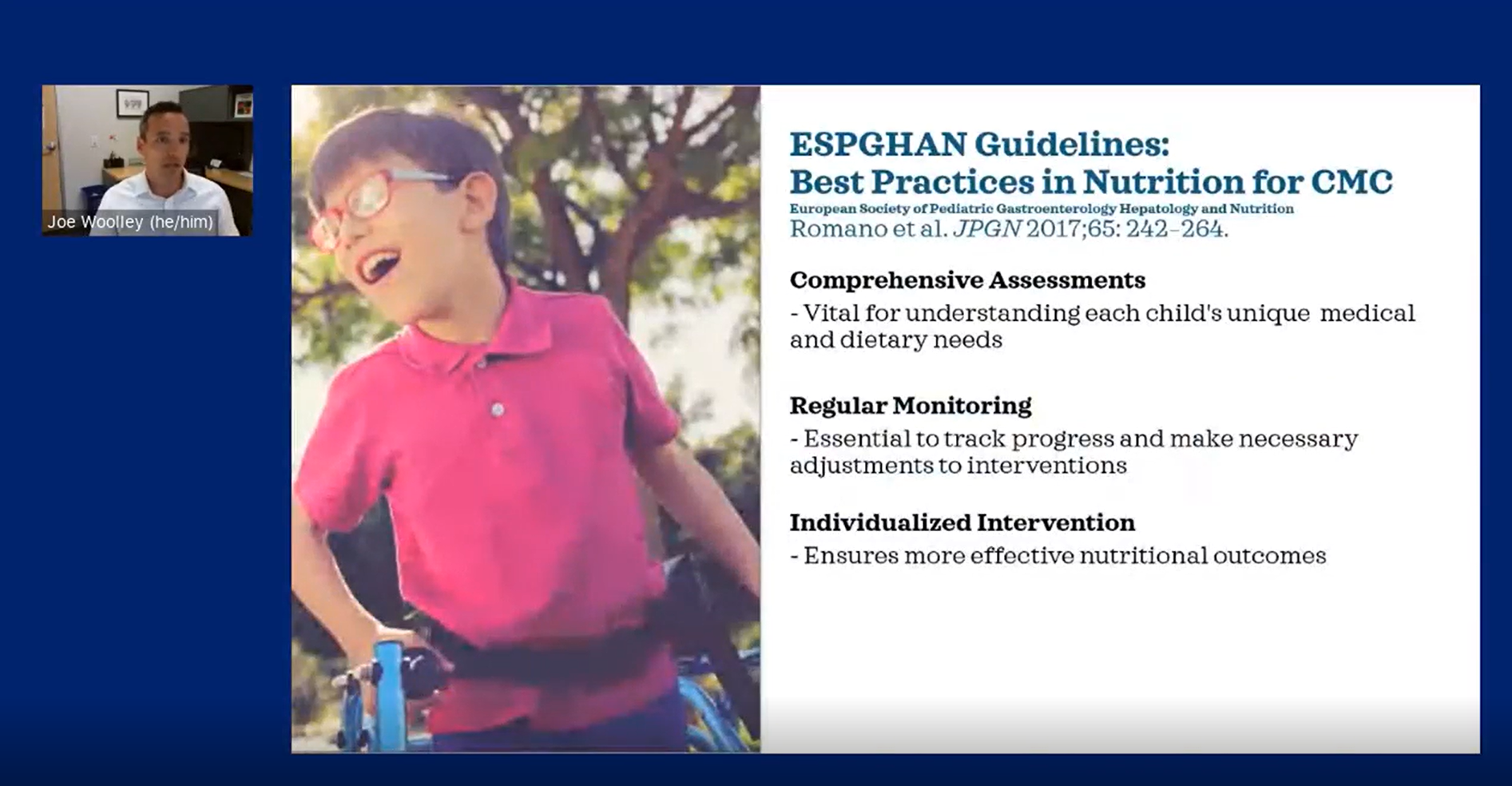
Determining whether a pediatric patient may need EN involves collaborative discussions between the child’s caregivers, the child (if appropriate), and multiple healthcare professionals, often including pediatricians, gastroenterologists, registered dietitians and other specialists involved in the child’s care.
Some medical conditions that prevent children from eating orally include:
- Weight loss or poor weight gain (resulting in failure to thrive and/or malnutrition) or severe lack of appetite
- Feeding and swallowing disorders or developmental delays
- Food allergies
- Cancer
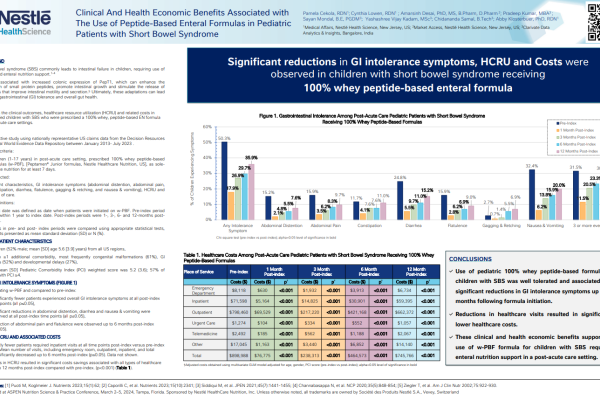
- Gastrointestinal issues such as an obstructed bowel, short bowel syndrome, or Crohn’s disease
- Gastroesophageal reflux disease (GERD) or esophagitis
- Cystic fibrosis (CF)
- Neurological disorders including paralysis
- Recovery from surgery or trauma
- Other acute and critical illnesses
Once the decision to place a feeding tube is made, an appropriate tube feeding formula is then selected to meet the child's individual needs to promote tolerance and support growth and development.
The types of feeding tubes used to administer enteral formulas are2:
- Nasogastric tube (NG-tube)
- Gastrostomy tube (G-tube)
- Jejunostomy tube (J-tube)
Ongoing collaboration between the child’s healthcare team, including pediatricians/pediatric gastroenterologists, dietitians, physician’s assistants, nurses/nurse practitioners, and speech-language pathologists, is key to managing a pediatric patient’s feeding tube and optimizing the child’s overall well-being and growth.
Nutrition For Tube-Fed Children
Choosing the right type of nutrition or specific formula for pediatric patients is critical to meeting their nutritional requirements and supporting their overall health and growth. Each child will have their own unique nutritional needs depending on multiple factors, such as age, weight, growth, medical conditions, neurological factors, and developmental stage.
Collaboration between the child’s caregivers and healthcare professionals, including registered dietitians, pediatricians, physician’s assistants, nurses, and speech/language pathologists, is important to select the most suitable formula. The specific formula selected for enteral feeding should provide an appropriate balance of macronutrients (carbohydrates, proteins, fats, fiber) and essential micronutrients (vitamins and minerals).
Considering the lifestyle and quality of life of parents and others caring for their children is also important.3 Ideally, families will have access to options that are convenient, readily available, and promote a positive feeding experience for both the child and their caregivers.
PEDIATRIC TUBE FEEDING FORMULAS
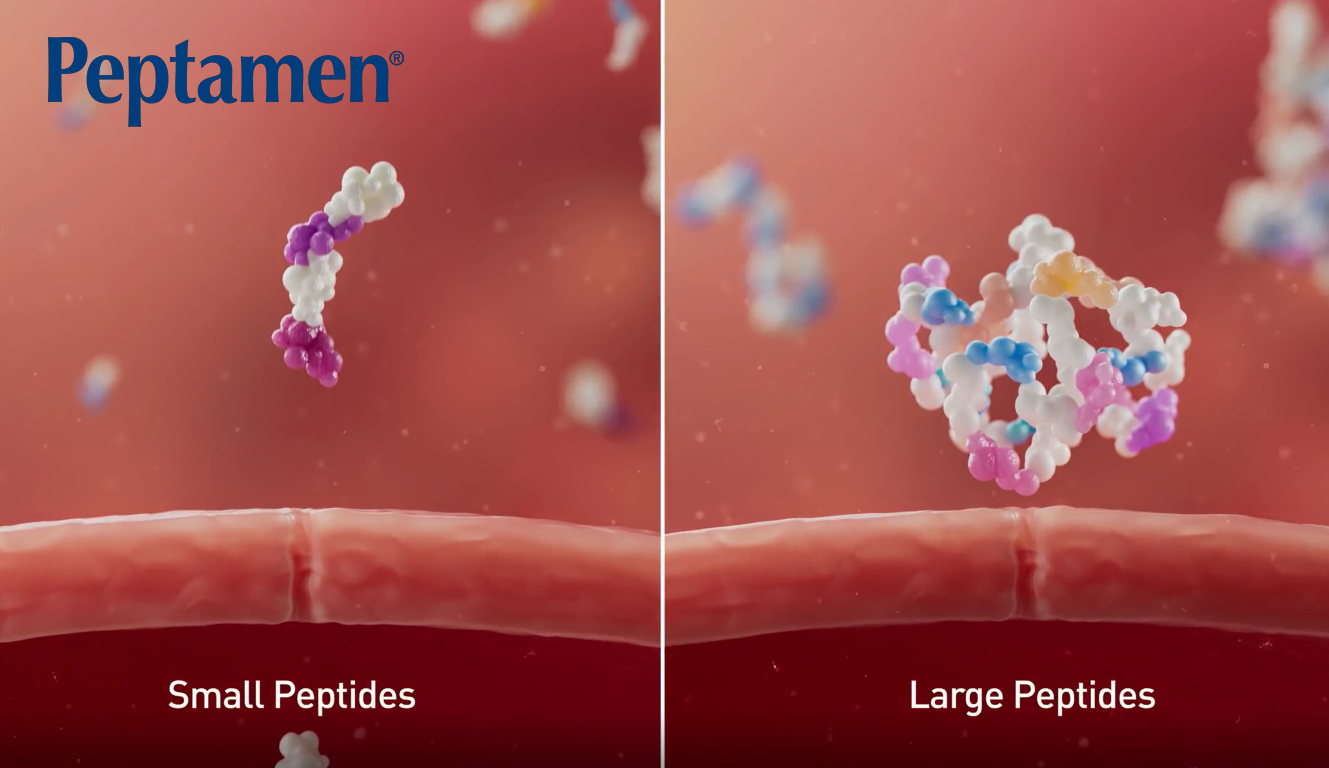
There are several types of tube feeding formulas available to meet the unique needs of tube-fed children. Most can tolerate a standard intact protein formula4. However, there are situations in which a standard formula may not be tolerated, or a patient has certain dietary requirements or preferences, and options should be considered.
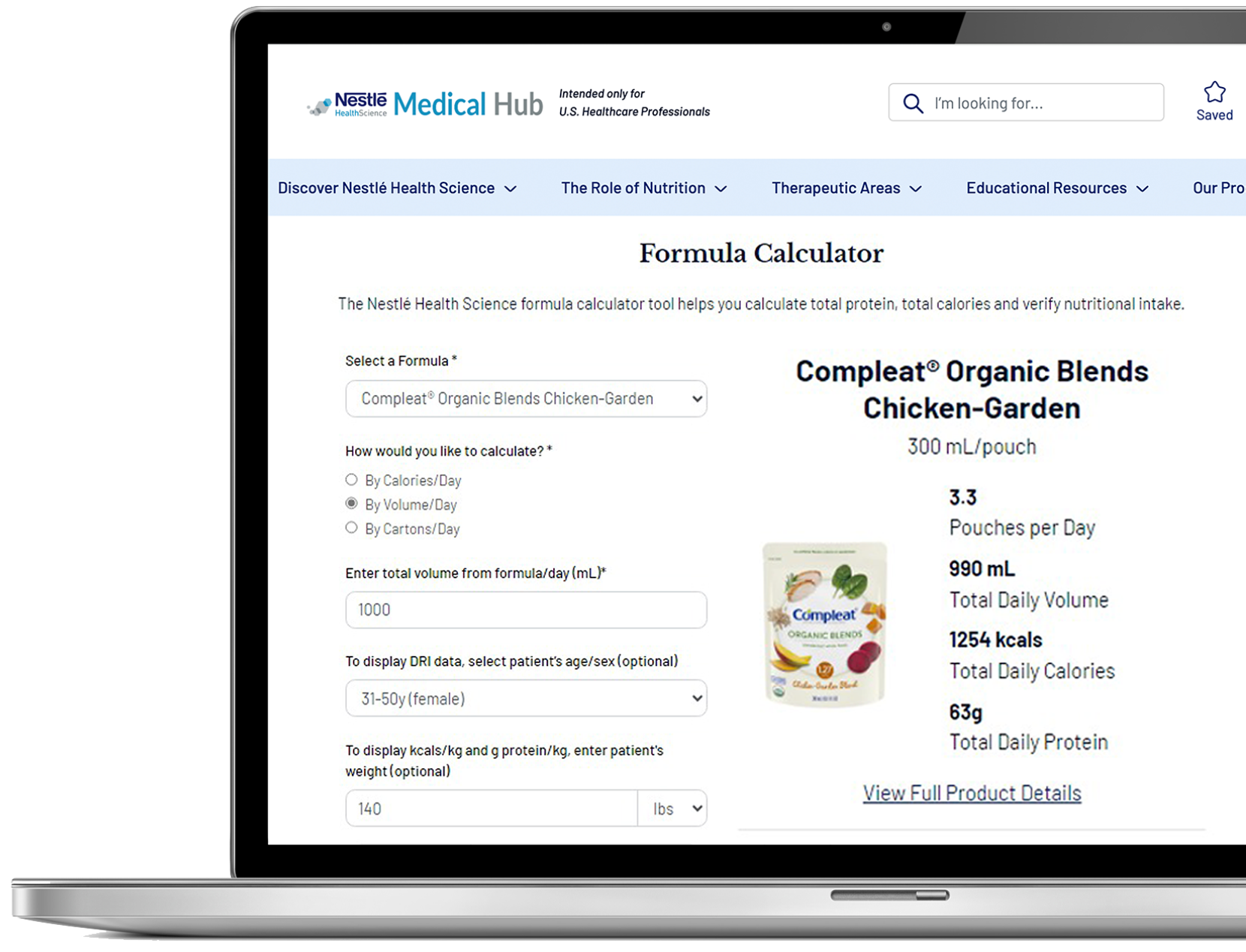
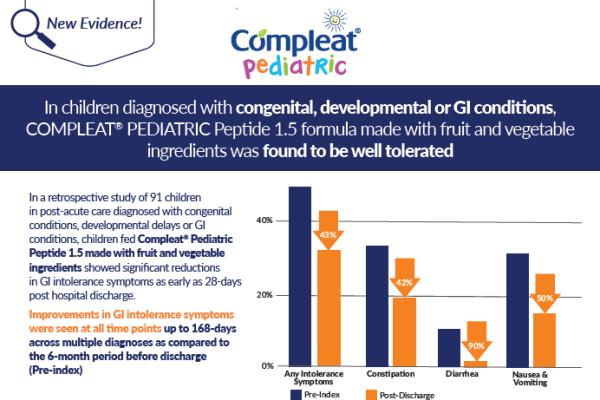
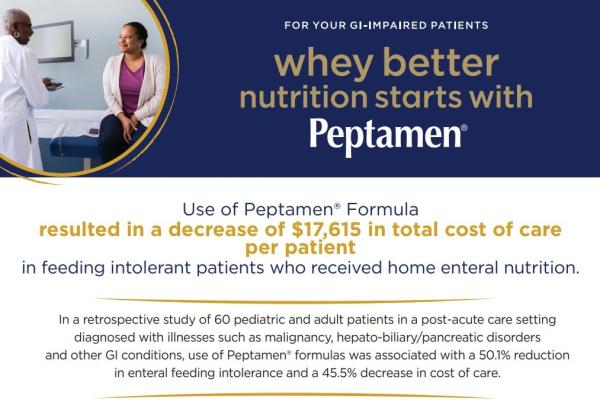
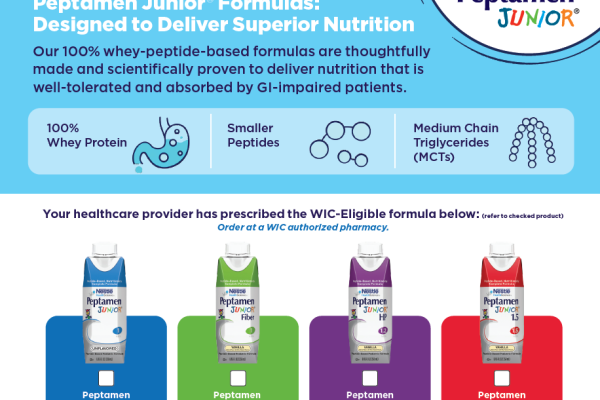
Nestlé Health Science offers a comprehensive portfolio of high-quality, evidence-based enteral tube feeding formulas to meet the unique needs of pediatric patients. Our portfolio includes standard formulas for normal digestion, peptide-based formulas for easier digestion and absorption, hypoallergenic formulas for food allergies and sensitivities, formulas with food ingredients for variety and tolerance, and commercially blenderized whole food formulas for a more natural feeding experience. These formulas meet the highest standards of nutritional quality, supporting optimal growth, development, and overall improved outcomes.
Support Resources
You must be logged in to view all resources.
12 Evidence Found
12 Tools and Product Support Found
8 Patient Resources Found
16 Videos
References
1. https://www.merckmanuals.com/professional/nutritional-disorders/nutritional-support/enteral-tube-nutrition
2. https://www.nutritioncare.org/about_clinical_nutrition/what_is_enteral_nutrition/
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5788946/
4. McClave SA, Taylor BE, Martindale RG, et. Al., Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient; Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr 2016;40:159-211.
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6575127/#:~:text=the%20feeding%20tube.-,Blenderized%20tube%20feeding%20(BTF)%20is%20defined%20as%20the%20use%20of,Table%201)%
6. Bobo E. Reemergence of blenderized tube feedings: exploring the evidence. Nutr Clin Pract. 2016;31(6):730–735. doi: 10.1177/0884533616669703.
7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9103110/
8. Henrikson A et al. Chronic Conditions in Children Receiving Commercially Blenderized Tube Feeding Formula in the Post-Acute Care Setting: Real World Evidence of Clinical and Health Economic Outcomes. J Parenter Enteral Nutr.2023;47(S2):S218.
9. From 2017 publication in NCP: Mundi MS. “Prevalence of Home Parenteral and Enteral Nutrition in the United States https://aspenjournals.onlinelibrary.wiley.com/doi/full/10.1177/0884533617718472