About Pediatric Impaired GI Function
The digestive system is made up of the gastrointestinal (GI) tract (the mouth, esophagus, stomach, large and small intestines, and anus) and the liver, pancreas, and gallbladder. In digestion, food and drink are broken down into small parts (called nutrients) that the body can absorb and use as energy and building blocks for cells.
The principal functions of the GI tract are to digest and absorb ingested nutrients, and to excrete waste products of digestion.11 The breakdown of complex macromolecules in foods to simple absorbable components is accomplished by the digestive system in four steps:
- ingestion,
- the mechanical and chemical breakdown of food,
- nutrient absorption, and
- elimination of indigestible food.
These absorbable components are processed by cells throughout the body and converted into energy or are used as building blocks.
GI disorders can affect different parts of the GI tract, mainly gastric or intestinal routes. Depending on the cause, severity and chronicity, an impaired GI function can alter food absorption and/or digestion, where the digestive tract is unable to effectively digest and absorb nutrients from food, affecting the overall nutritional status and health of the child.5-7
Childhood is a time of rapid growth (anabolism), and this stage of life needs to be properly fueled by essential nutrients. Digestive disorders and other health challenges can make it difficult to meet nutrition needs. If any section of the GI tract is impaired due to inflammation, blockages or other issues, nutrient malabsorption or maldigestion may occur, which may lead to nutritional deficiencies.
Symptoms of GI impairment may include constipation, diarrhea, upset stomach, abdominal pain, bloating, gas and vomiting. Some disorders that may cause GI impairment include:
- Gastro-esophageal Reflux Disease (GERD)
- Acute or Chronic Diarrhea
- Constipation
- Cow or Soy Milk Allergy/Intolerance
- Cerebral Palsy (CP)
- Celiac Disease (CD)
- Irritable Bowel Disease (IBD)
- Short Bowel Syndrome (SBS)
Children with impaired GI function are at risk for malnutrition and reduced quality of life.12 It is for this reason that a specific focus is placed on the nutritional status of these children, as optimum nutrient intake has been shown to support normal growth and development as well as improve overall health and quality of life.12
At Nestlé Health Science, we are committed to providing nutritional therapies that are tailored to the individual needs of the child. In the case of infants and children with GI impairment, these needs are very specific to the condition, which is why we have a range of different solutions to fulfill a variety of nutritional requirements, including enteral (tube-feeding) nutrition formulas and oral nutritional supplements suitable from infancy through adolescence.
Nutrition & Pediatric Impaired GI Function
The type of nutritional support required for pediatric impaired GI function is as varied as the underlying causes and presentations of symptoms. Among the more common conditions associated with impaired GI function include:13,14
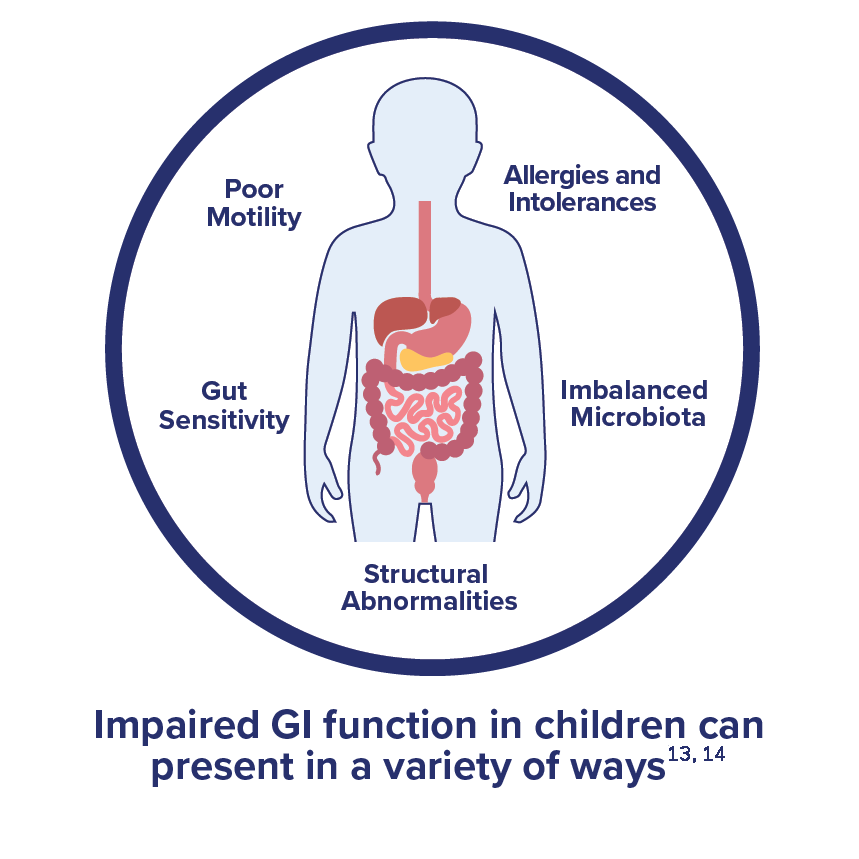
- Poor motility, often leading to constipation or reflux. Nutrition strategies may be used to allow for better ease of movement down the GI tract and prevent slowdowns or stoppages.
- Altered gut sensitivity, as seen in cases of irritable bowel syndrome or anxiety. The key is to find nutritional solutions that can be tolerated along with other treatments the patient may require.
- Imbalance of gut microbiota, especially if the patient is on antibiotics. Probiotic-containing formulas help restore colonies of helpful gut microbes.
- Allergies and intolerances, leading to poor nutrient absorption. Patients may need allergen-free or elemental formulas to deliver necessary nutrients.
- Structural abnormalities, such as short gut syndrome. Enteral feeding and nutrition solutions are often required in these cases, especially if portions of the gut have been removed or are blocking areas in which nutrient absorption would ordinarily occur.
Finding the right nutritional strategies to help children with impaired GI function can go a long way toward improving patient outcomes and enabling children to continue growing and thriving.14 Nestlé Health Science has a number of pediatric nutrition formulas for both enteral and oral use that have been clinically tested to provide positive clinical outcomes to children that need them.
Support Resources
You must be logged in to view all resources.
16 Evidence Found
19 Tools and Product Support Found
References
- Kliegman RM. Digestive system disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 123.
- Van de Heijning BJM, et al. GI symptoms in infants are a potential target for fermented infant milk formulae: a review. Nutrients 2014; 6: 3942-67.
- Iacono G, et al. Gastrointestinal symptoms in infancy: a population-based prospective study. Dig Liver Dis 2005; 37: 432-8.
- Goday PS. Gastrointestinal disorders: Red flags and best treatments. Contemporary Pediatrics. July 2021: 16-19. https://www.contemporarypediatrics.com/view/gastrointestinal-disorders-red-flags-and-best-treatments.
- Romano C, et al. European Society for Paediatric Gastroenterology, Hepatology and Nutrition Guidelines for the evaluation and treatment of gastrointestinal and nutritional complications in children with neurological impairment. J Pediatr Gastroenterol Nutr 2017;65(2):242-64.
- Huysentruyt K, et al. Nutritional red flags in children with cerebral palsy. Clin Nutr 2019 Mar 8. pii: S0261-5614(19)30094-9.
- Miele E, et al. Nutrition in Pediatric Inflammatory Bowel Disease: A Position Paper on Behalf of the Porto Inflammatory Bowel Disease Group of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2018;66(4):687-708.
- Nestle Health Science press release: Nutritional management of children with gastrointestinal Impairment – key to clinical outcome; Presentation at ESPHGAN meeting, May 29, 2013. https://www.nestlehealthscience.com/newsroom/press-releases/Espghan-2013
- Kay M., Tolia V. Common gastrointestinal problems in pediatric patients. American College of Gastroenterology. http://s3.gi.org/patients/gihealth/pdf/pediatric.pdf. Accessed 9/9/2023.
- Gastrointestinal Challenges in the Neurologically Impaired Child (nestlenutrition-institute.org). Accessed 9/9/2023.
- Hornbuckle WE, Simpson KW, Tennant BC. Gastrointestinal Function. Clinical Biochemistry of Domestic Animals. 2008:413–57. doi: 10.1016/B978-0-12-370491-7.00014-3. Epub 2008 Oct 22. PMCID: PMC7173558.
- Varni JW, Bendo CB, Nurko S, Shulman RJ, Self MM, Franciosi JP, Saps M, Pohl JF; Pediatric Quality of Life Inventory (PedsQL) Gastrointestinal Symptoms Module Testing Study Consortium. Health-related quality of life in pediatric patients with functional and organic gastrointestinal diseases. J Pediatr. 2015 Jan;166(1):85-90. doi: 10.1016/j.jpeds.2014.08.022. Epub 2014 Sep 17. PMID: 25241177.
- Gastrointestinal Diseases. Cleveland Clinic Health Library. https://my.clevelandclinic.org/health/articles/7040-gastrointestinal-diseases. Accessed 9/9/2023.
- Fikree A, Byrne P. Management of functional gastrointestinal disorders. Clin Med (Lond). 2021 Jan;21(1):44-52. doi: 10.7861/clinmed.2020-0980. PMID: 33479067; PMCID: PMC7850201.