Transition to Peptide Based Formula is Associated with Greater Tolerability and Reduction in Healthcare Utilization in Children Receiving Enteral Nutrition
Elfadil OM, Steien D, Narasimhan R, Epp L, Velapati S, Patel I, Patel J, Hurt R, Mundi M.
Journal of Parenteral and Enteral Nutrition 2021;1-9. DOI:10.1002/jpen.
Introduction:
Prevalence of home enteral nutrition (HEN) has increased significantly over the past few decades. Enteral feeding intolerance (EFI) is a frequent cause of suboptimal nutrition in children on HEN and is defined as the presence of gastrointestinal (GI) distress, significant gastric residual volume and suboptimal delivery of enteral nutrition (EN).
Objective:
The purpose of this study was to assess changes in GI tolerance and healthcare utilization in children receiving peptide-based HEN (PBD).
Methods:
This was a retrospective review of the electronic medical records of children <18 years of age and receiving at least 80% of nutrition needs from EN between October 2015 and October 2019.
Results:
A total of 30 children participated, 21 (70%) of whom were directly started on PBD as an initial formula (PBD-i) and 9 (30%) who were initiated on a standard polymeric formula (SPF) and later transitioned to a PBD (PBD-t). 66.7% of participants were male with a mean age of 8.4 years in the PBI-i group and 10.2 years in the PBD-t group. Indications for use of enteral nutrition (EN) included malnutrition, dysphagia, poor oral intake/feeding difficulties and bridge to oral feeding. Indications for use of PBD included malnutrition, pancreatic insufficiency, and current or past intolerance to SPF.
Patients receiving PBD-i were on their formula for a median of 37 weeks with a median weight gain of 2.6 kg. Those receiving PBD-t were on PBD for a median of 22 weeks and experienced median weight loss of 0.5 kg while on SPF, and median weight gain of 2.7 kg while on PBD. Patients were able to consume 94.8% of goal energy needs from PBD, as compared to 73.3% from SPD formulas. After transition to PBD, no symptoms were reported in 6 of 9 patients (66.7%).
Figure 1 shows the reduction in GI distress with a transition to PBD (P=0.45)
Figure 2 shows that healthcare utilization also significantly declined after transition to PBD.
Conclusion:
In children who required long-term HEN, PBD was well-tolerated as either an initial HEN formula or as a transition feeding. In SPF-intolerant children, transition to PBD resulted in significant improvement in HEN tolerance and a reduction in healthcare utilization.
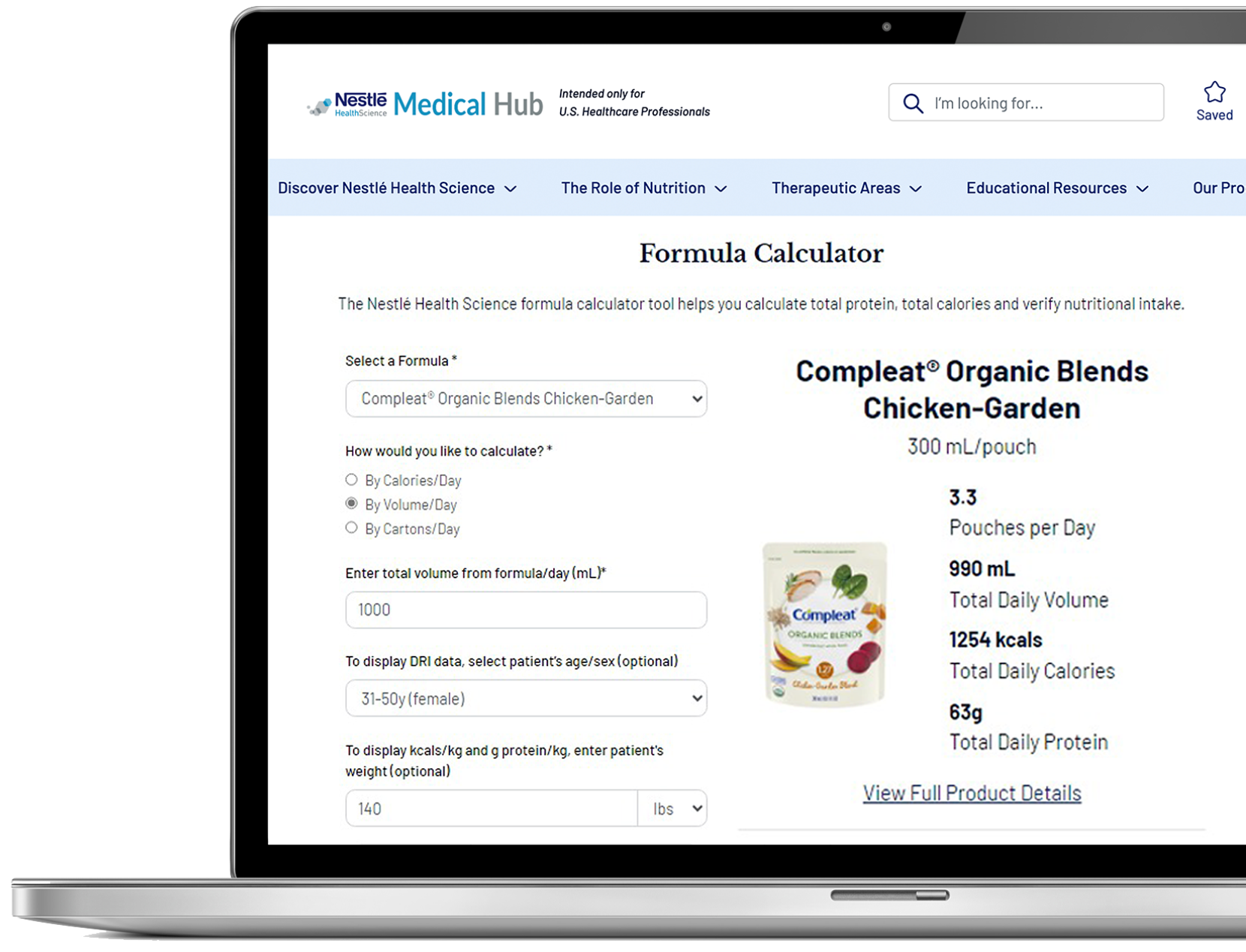
Abstract Summary Prepared by Nestlé Health Science. Download PDF of Summary
The published abstract can be accessed at: https://aspenjournals.onlinelibrary.wiley.com/doi/epdf/10.1002/jpen.2202
©2021 Nestlé. All rights reserved.