Malnutrition
Malnutrition
Malnutrition can lead to and worsen acute and chronic medical conditions, especially among older adults. The consequences of malnutrition are serious: it increases the risks for complications; leads to longer hospital length of stay and hospital readmissions, leading to higher healthcare costs; and is associated with increased risk of mortality and morbidity. Malnutrition decreases quality of life, functional status, activities of daily living, wound healing, muscle mass and strength.2-4
And, the economic burden of malnutrition is high: disease-associated malnutrition creates a $157 billion burden in the U.S. annually, considering direct medical costs, quality-adjusted life years lost, and mortality8; direct medical costs of disease-associated malnutrition total $15.5 billion annually in the U.S.3; the 30-day readmission rate is more than 50% higher, and the average cost per readmission is 26% higher for patients with malnutrition compared to patients without malnutrition.2
Nestlé Health Science offers a range of nutrition solutions to help improve health outcomes and quality of life for people with malnutrition and other related conditions.
Malnutrition
Malnutrition
Malnutrition can lead to and worsen acute and chronic medical conditions, especially among older adults. The consequences of malnutrition are serious: it increases the risks for complications; leads to longer hospital length of stay and hospital readmissions, leading to higher healthcare costs; and is associated with increased risk of mortality and morbidity. Malnutrition decreases quality of life, functional status, activities of daily living, wound healing, muscle mass and strength.2-4
And, the economic burden of malnutrition is high: disease-associated malnutrition creates a $157 billion burden in the U.S. annually, considering direct medical costs, quality-adjusted life years lost, and mortality8; direct medical costs of disease-associated malnutrition total $15.5 billion annually in the U.S.3; the 30-day readmission rate is more than 50% higher, and the average cost per readmission is 26% higher for patients with malnutrition compared to patients without malnutrition.2
Nestlé Health Science offers a range of nutrition solutions to help improve health outcomes and quality of life for people with malnutrition and other related conditions.
Malnutrition
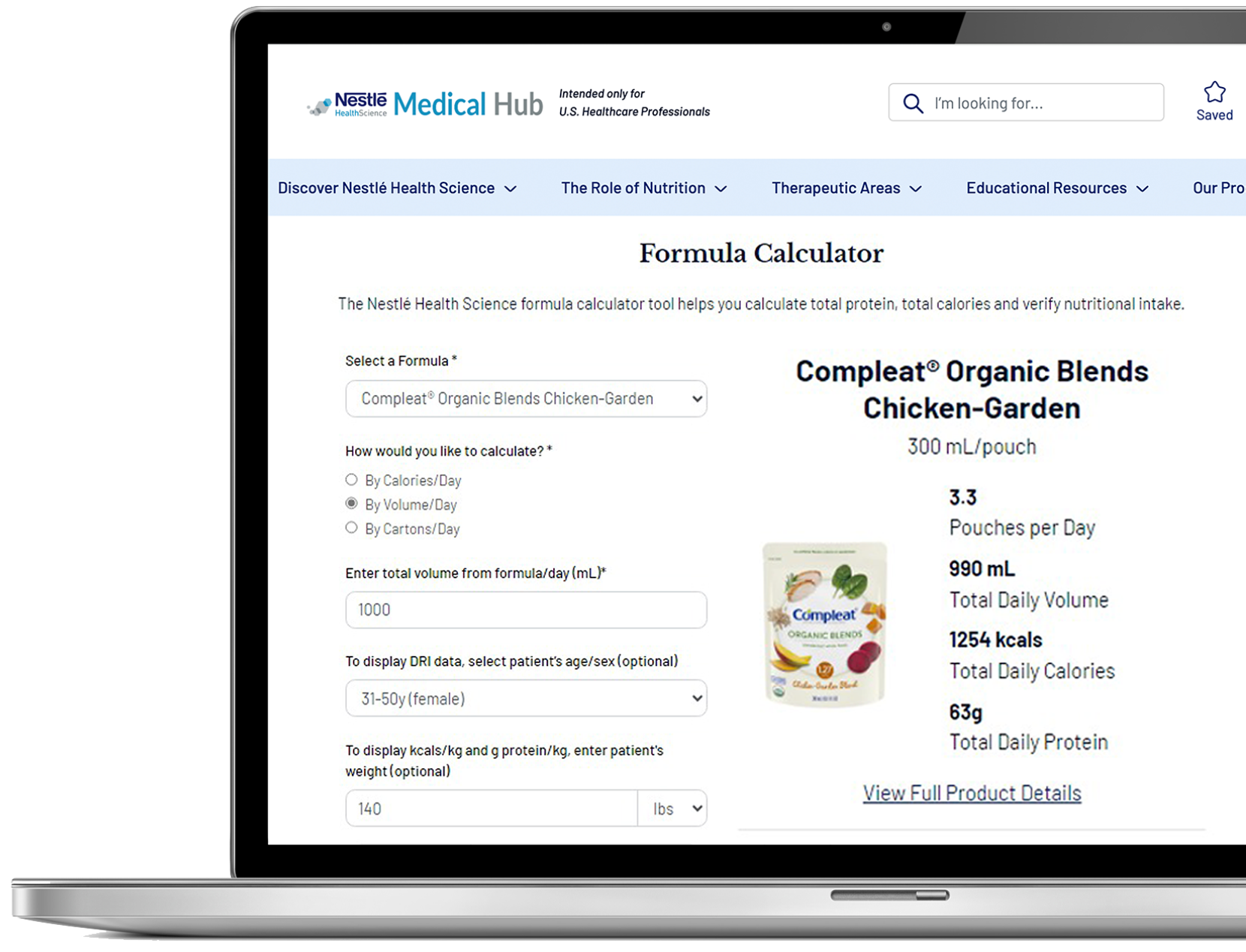
> Clinician Tools
1. https://www.modernhealthcare.com/article/20160923/NEWS/160929940/malnutrition-causes-15-5-billion-in-healthcare-spending-per-year
2. Fingar KR et al. Healthcare Cost and Utilization Project. 2016; Statistical Brief #218.
3. Goates S et al. PLoS One. 2016;11:e0161833.
4. Snider JT et al. JPEN. 2014;38(2 Suppl):77S-85S.
5. https://www.who.int/news-room/fact-sheets/detail/malnutrition
6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4951875/
7. Eckert KF, Cahill LE. Malnutrition in Canadian hospitals. CMAJ 2018;190:E1207.
8. Snider JT et al. JPEN. 2014;38(2 Suppl):77S-85S.
9. Dehghankar L et al. Biotech Health Sci. 2016;3:e34470.
10. Pierik VD, et al. BMC Geriatrics. 2017;17:118.
11. Liguori I et al. Nutr Clin Pract. 2018;33:879-886.
12. Dorner TE et al. J Nutr Health Aging. 2014;18:264-269.
13. Jacobsen EL et al. BMJ Open. 2016;6:e011512.
14. Neyens J et al. Arch Gerontol Geriatr. 2013;56:265-269.
15. Kaiser MJ et al. J Am Ger Soc. 2010; 58:1734-1738.
16. Malnutrition: Definition, Causes, Symptoms & Treatment (clevelandclinic.org)
17. Bauer J et al. J Am Med Dir Assoc. 2013;14:542-559.
18. Deutz NEP et al. Clin Nutr. 2014; 33:929-936.
19. Krok-Schoen J et al. J Nutr Aging. 2019; Feb 19 (Epub ahead of print).
20. Cawood AL et al. Ageing Res Rev. 2012;11:278-296.
21. Donini, Lorenzo M., et al. J Nutr Health Aging vol. 17, no. 1, 2012; 9-15.