About Critical Care
Critical care refers to a specialized branch of medicine that focuses on the comprehensive care of acutely ill patients who are facing life-threatening conditions. These patients require close and constant monitoring, often in an intensive care unit (ICU) setting, due to the severity of their illness or injury. Critical care professionals, such as intensivists, nurses, and respiratory therapists, play a vital role in providing immediate and intensive medical intervention, utilizing advanced technologies and interventions to stabilize and support patients' organ systems.
Nutrition support is an important aspect of the management of critically ill patients. These patients often experience significant metabolic stress and are at an increased risk of malnutrition due to their illness or injury.3 Appropriate nutrition is essential to support the body's metabolic requirements, promote wound healing, maintain organ function, and enhance immune response.4,5,6,7,11
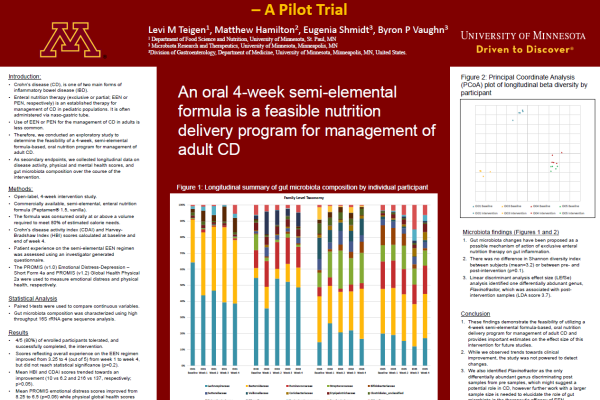
Nutrition in critical care involves the careful assessment of each patient's nutritional needs, including conditionally essential macronutrients (proteins, carbohydrates, and fats) and micronutrients (vitamins and minerals), and the development of individualized feeding protocols. This may involve specialized enteral nutrition, where condition-specific nutrients are provided through a tube into the gastrointestinal tract, or parenteral nutrition, where nutrients are delivered intravenously. Close collaboration between healthcare professionals, including dietitians, physicians, nurses, and pharmacists is crucial to ensure optimal nutrition for patients in the critical care setting, and to ultimately help support their recovery and outcomes.
Nutrition & Critical Care
NUTRITION IN A CRITICAL CARE SETTING
Appropriate nutritional support plays a pivotal role in the treatment of patients in a critical care setting, as it directly impacts their overall recovery and outcomes. Critically ill patients often experience a heightened metabolic stress response and are at risk of developing malnutrition. Providing appropriate and timely personalized nutrition is crucial to meet increased metabolic demands, promote tissue repair, maintain organ function, and support immune function.
Studies have demonstrated that providing appropriate and timely nutrition to adults in critical care settings can have significant benefits. A prospective study examining the effects of early enteral nutrition (within 48 hours) versus late enteral nutrition in medical ICU patients showed a 21% decrease in mean hospital length of stay and a 24.5% decrease in mortality in those patients receiving early enteral nutrition.8
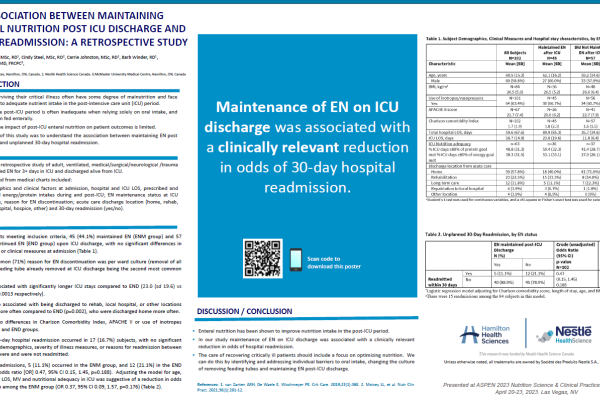
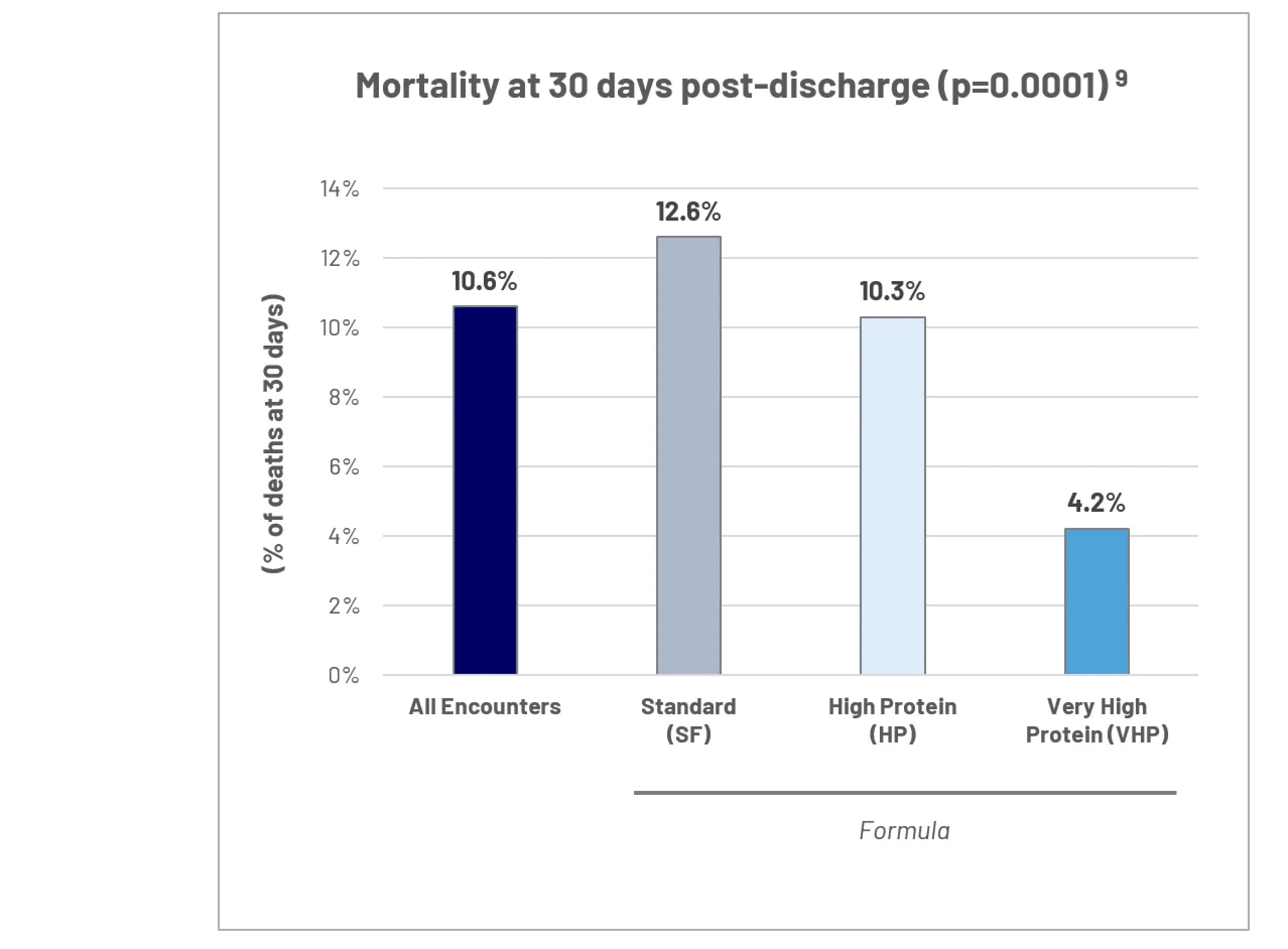
In a retrospective analysis of 2000 ICU patient encounters in the Geisinger health care system, there was a decrease 30-day post-discharge mortality associated with utilization of a progressive delivery of a very high protein, low carbohydrate formula during the first seven days of critical illness.9 Appropriate nutrition therapy improves clinical outcomes and optimizes resource utilization.
NUTRITIONAL STRATEGIES FOR CRITICAL CARE PATIENTS
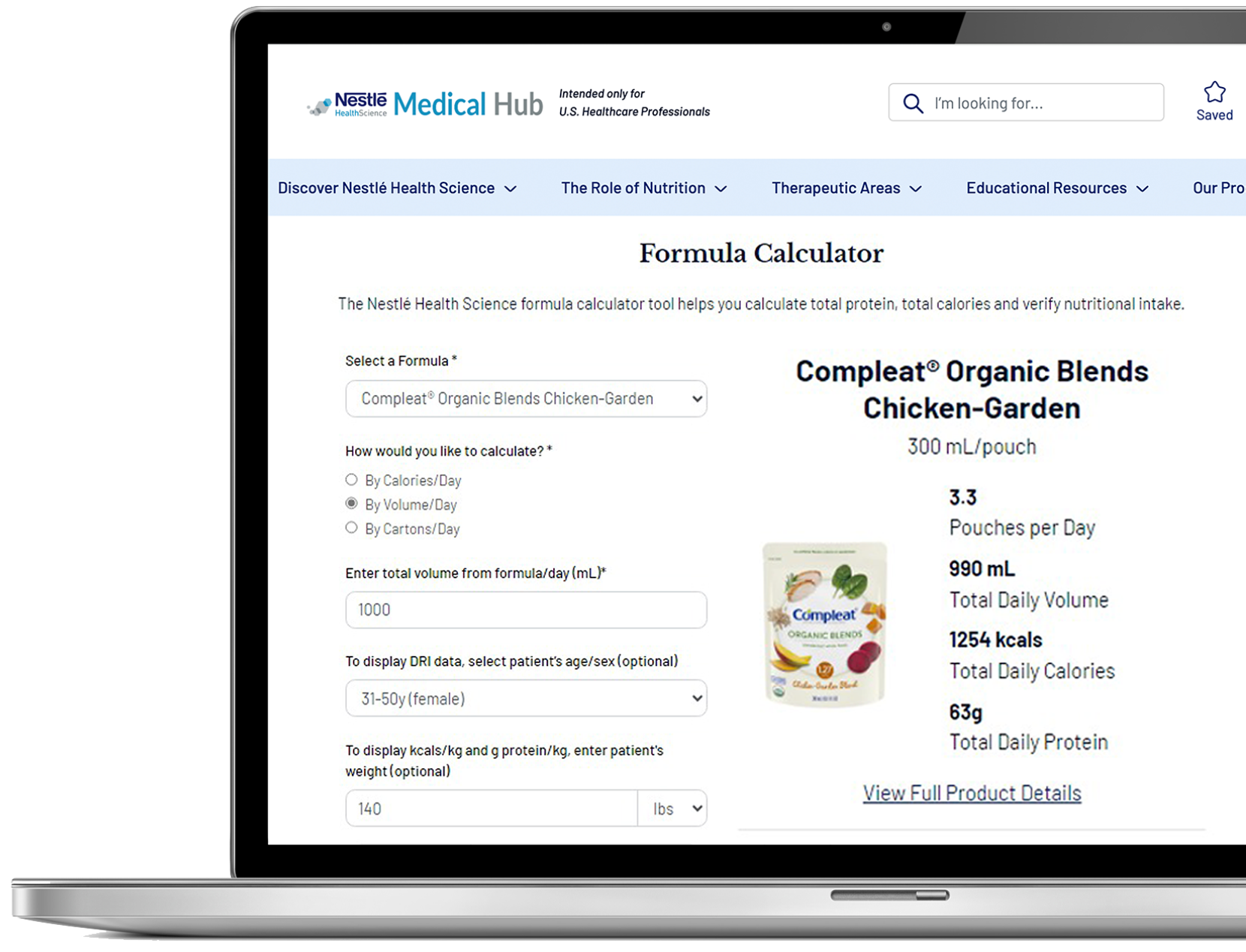
In the critical care setting, nutritional strategies are tailored to the individual needs of each patient, as there is no one-size-fits-all approach. Patient assessment, including nutritional status, underlying medical conditions, and the severity of illness, is essential to determine the appropriate nutrition plan. This assessment is typically conducted by a multidisciplinary team, involving dietitians, physicians, nurses and pharmacists, who collaborate to design personalized feeding plans.
Enteral tube feeding may provide nutritional and non-nutritional benefits such as maintaining gut integrity, supporting immune response and increasing gut motility.10 Because of this, it may preferred over parenteral feeding (providing nutrition through the vein), whenever possible. However, in some cases, such as bowel obstruction, parenteral nutrition may be necessary.
Choosing the right nutrition for each patient is important, considering factors such as the patient's nutritional needs, underlying medical conditions, gastrointestinal tolerance, and specific requirements for protein, calorie, or disease-specific nutritional support. Ongoing monitoring and careful adjustment of the nutrition plan are essential to ensure optimal support throughout the patient's critical care journey.
Support Resources
You must be logged in to view all resources.
36 Evidence Found
26 Tools and Product Support Found
34 Videos
References
1. Dvir D, et al. Clin Nutr 2005;25:37-44.
2. Villet S, et al. Clin Nutrt 2005; 24:502-9.
3. Sharma K, et al. NCP 2019;34(1):12-22.
4. Wernerman J, et al. Critical Care 2019;23:318.
5. Singer P. Critical Care 2019;23(Suppl1):139.
6. Chu AS, et al. Adv Skin Wound Care 2021;34:630-6.
7. Aguilar-Nascimento JE, et al. Nutrition 2011;440-44.
8. Ghorabi S, Shariatpanahi Z. Thrita 2014;3(3):e20905.
9. Ochoa J, et al. Clin Nutr 2022;41:2833-2842.
10. McClave SA, et al. Crit Care Med 2014;42(12):2600-2610.
11. Prest PJ, et al. JPEN 2020;44(5):880-888.